Reduction of Risk Potencial / 05
Make sure to:
- Analyze the areas of quality and safety of care.
- Describe methods to prevent and reduce safety risks.
- Understand the importance of the application of patient safety recommendations and strategies.
 According to the World Health Organization (2020), quality of care refers to the extent to which healthcare services delivered to individuals and communities enhance the probability of attaining favorable health outcomes in alignment with evidence-based professional expertise. One of the areas that make up the quality of health services is safety and patient-centered care.
According to the World Health Organization (2020), quality of care refers to the extent to which healthcare services delivered to individuals and communities enhance the probability of attaining favorable health outcomes in alignment with evidence-based professional expertise. One of the areas that make up the quality of health services is safety and patient-centered care.
September 17 marks World Patient Safety Day, which is defined by the World Health Organization (2023) as "the absence of avoidable harm to a patient and the reduction of the risk of unnecessary harm associated with healthcare to an acceptable minimum". An adverse event, as defined by the Institute for Healthcare Improvement, is an unintentional physical harm caused by or linked to medical care, necessitating extra monitoring, treatment, hospitalization, or leading to fatality (Potter et al., 2021). Thus, patient falls, pressure ulcers, and medication errors are recognized as some of the most frequent adverse events occurring in healthcare institutions (World Health Organization, 2023).
The essence of nursing is caring with a focus on safety, which includes care that is humanized, based on evidence, and deliberately designed to support the process of meeting needs related to health situations and to protect clients. Protection includes support in the process of satisfying fundamental human needs in conditions of weakness or impossibility due to health causes, It involves the creation of means to guarantee the integrity, dignity and rights of people, the creation of conditions to free the environment from threats, risks and fear, and the proactive attitude to prevent possible adverse events.
4.1 Pressure Ulcers
 Nursing care plays a vital role in protecting patients by maintaining skin integrity and preventing pressure ulcers. Most pressure lesions are preventable, through a continuous assessment of the patient's skin condition, which allows the application of preventive measures to avoid them.
Nursing care plays a vital role in protecting patients by maintaining skin integrity and preventing pressure ulcers. Most pressure lesions are preventable, through a continuous assessment of the patient's skin condition, which allows the application of preventive measures to avoid them.
Pressure ulcers are caused by ischemia. Tissue is compressed between the bed or chair and the bony prominences. In the event of ischemia, cells experience a lack of oxygen and nutrients, leading to the accumulation of metabolic waste products and eventual tissue death (Berman et al., 2022). In dark-skinned clients, these features may be difficult to detect. To find out if there is skin alteration, the reactions of the explored areas should be compared with other parts of the client's skin. If, when pressure is released, the redness disappears, there is no tissue damage; if, on the other hand, the redness does not disappear, tissue damage has occurred (Berman et al., 2022).
All hospitalized patients are at risk of skin lesions. This risk increases with immobility, reactions to various medications, and wetness due to incontinence or festering wounds, as well as neurological deficiencies, chronic diseases, inadequate nutrition, decreased mental status, low cardiac output, poor tissue oxygenation, or orthopedic and vascular injuries. Also at risk are patients who are homebound, in nursing homes or long-term care facilities, depending on their level of mobility and chronic comorbidities (Potter et al., 2021).
Several tools are available to assess pressure ulcer risk, such as the Braden Scale. This scale is made up of six subscales: sensory perception, moisture, activity, mobility, nutrition, and friction and shear. The maximum possible grade is 23 points. A score below 18 or 19 points is a risk for the patient. For the best results, nursing staff should be trained in the proper use of the scale.
Table 1
Risk Factors for Pressure Sores
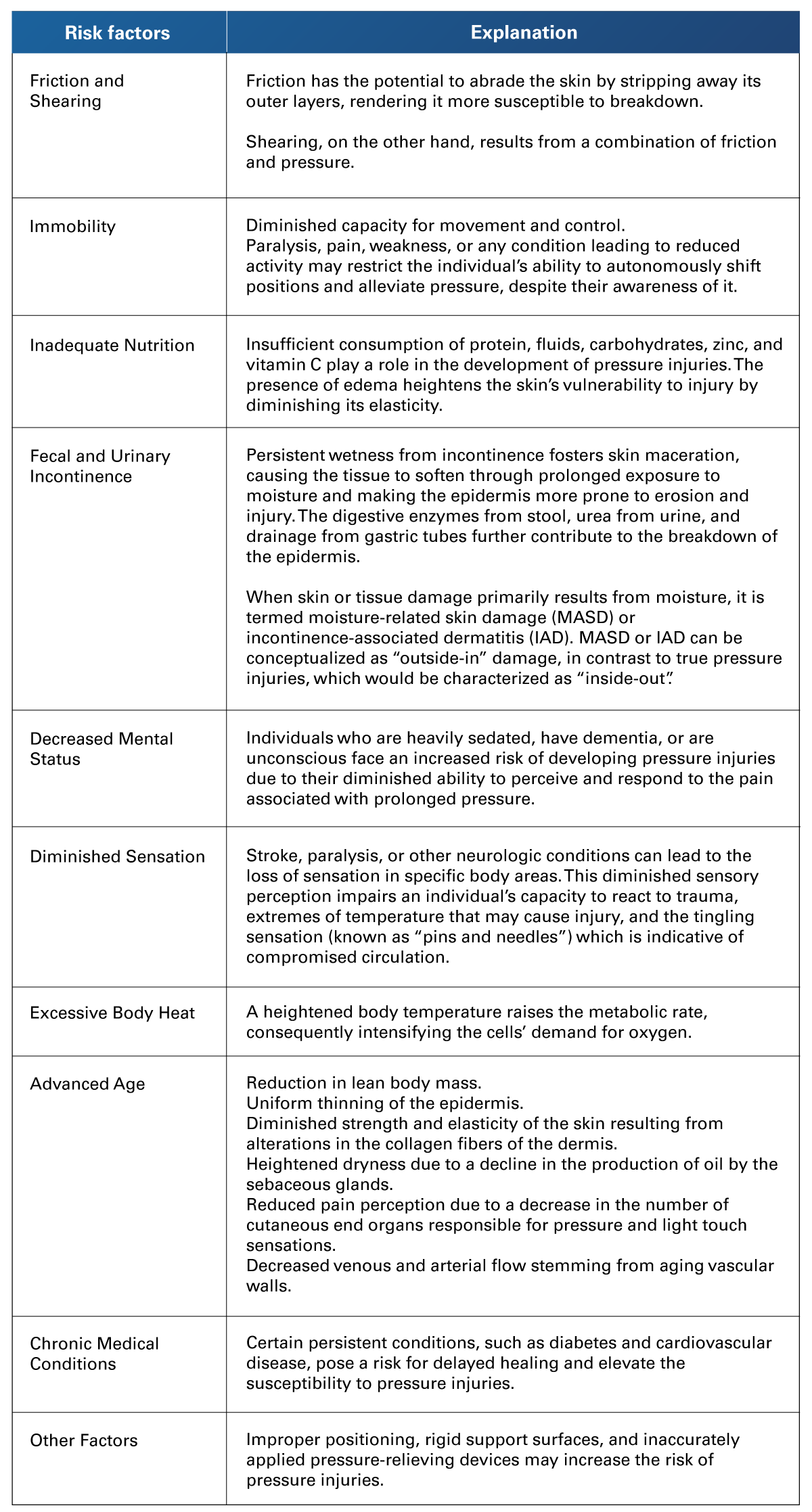 Adapted from Berman et al. (2022). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice. (11th ed.). Pearson Education Limited.
Adapted from Berman et al. (2022). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice. (11th ed.). Pearson Education Limited.
Table 2
Braden Scale for Risk of Pressure Sores
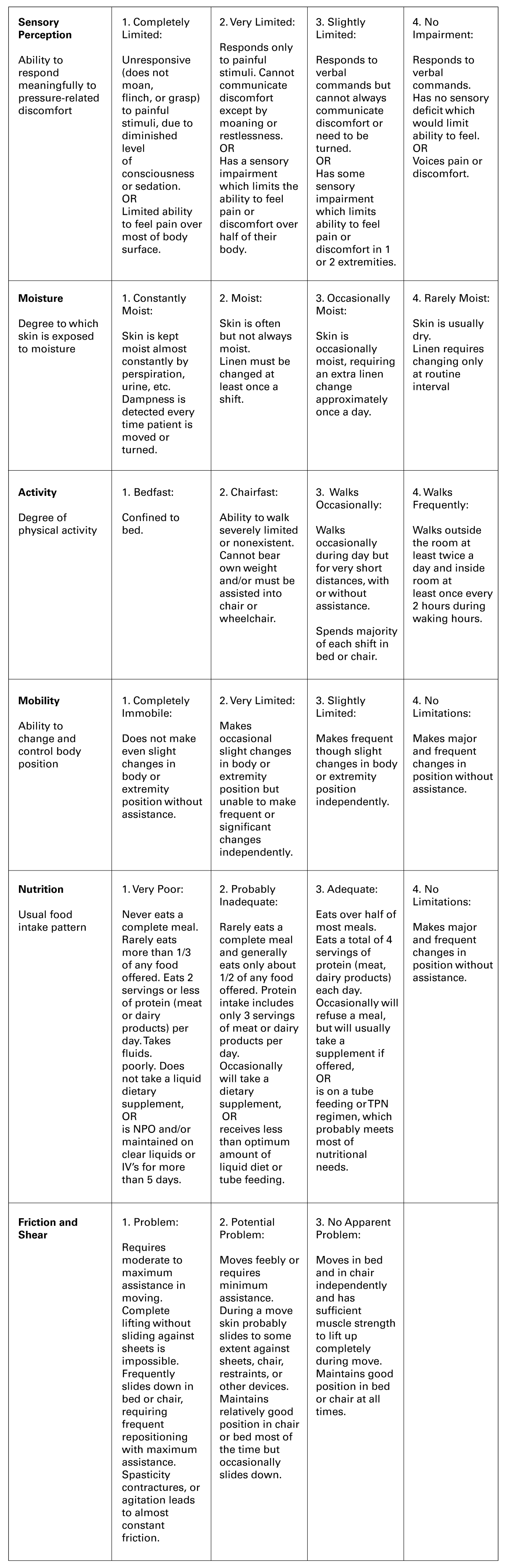 Adapted from Berman et al. (2022). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice. (11th ed.). Pearson Education Limited.
Adapted from Berman et al. (2022). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice. (11th ed.). Pearson Education Limited.
To prevent pressure or moisture ulcers, the nurse must use a variety of measures to maintain skin integrity. Two main steps are described in prevention: identifying at-risk clients and applying reliable prevention strategies to them. This means that the nurse performs a patient risk assessment upon admission and reassesses the risk of all hospitalized patients on a daily basis.
Table 3
Preventive Measures for Pressure Sores
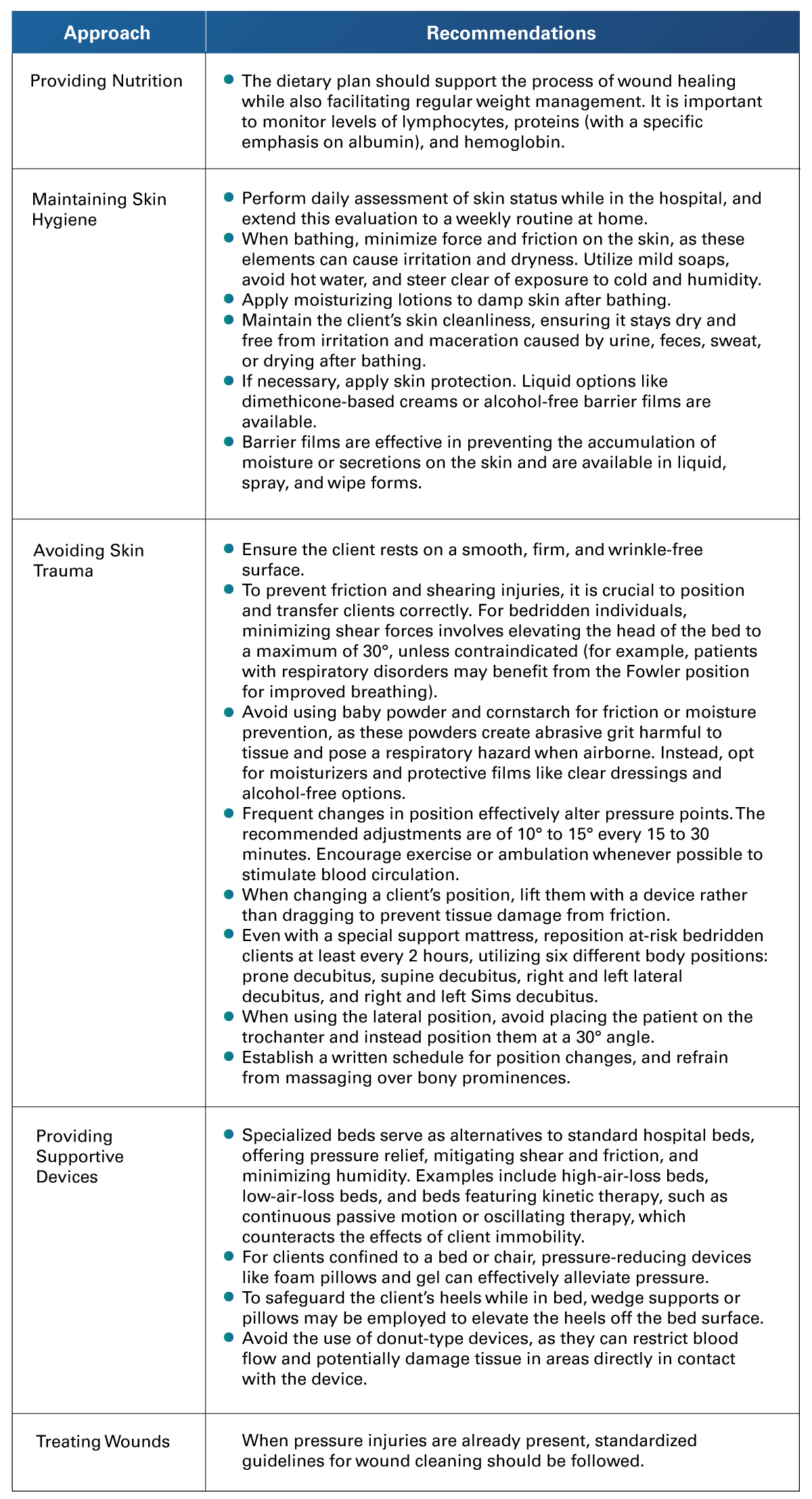 Adapted from Berman et al. (2022). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice. (11th ed.). Pearson Education Limited.
Adapted from Berman et al. (2022). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice. (11th ed.). Pearson Education Limited.
4.2 Fall Risk Prevention
 Falling is a risk for patients of all ages, but infants and older adults are especially prone to falls and serious injuries. As they age, older people's muscle strength decreases, which affects their balance and increases the risk of falls. 95% of hip fractures are due to falls, and they are the most frequent reason for hospital admission (Berman et al., 2022).
Falling is a risk for patients of all ages, but infants and older adults are especially prone to falls and serious injuries. As they age, older people's muscle strength decreases, which affects their balance and increases the risk of falls. 95% of hip fractures are due to falls, and they are the most frequent reason for hospital admission (Berman et al., 2022).
Falls are a significant safety concern, as they commonly cause functional dependence in elderly patients. This can lead to a fear of further falls, causing them to miss out on their usual activities, which contributes to a general loss of independence, possible hospitalization or admission to a long-term care facility (Potter et al., 2021).
According to Potter et al. (2021), falls are attributed to a combination of individual and environmental factors. Individual factors encompass impaired vision, cardiovascular issues (like postural hypertension or syncope), conditions influencing mobility (such as arthritis, muscle weakness, and foot problems), as well as those affecting balance. Other contributors include alterations in bladder function (like frequency or incontinence), cognitive impairments, and adverse reactions to medications. Notably, certain medications, such as benzodiazepines and other hypnotics, can compromise an older individual’s central nervous system and impact their gait, thereby influencing the risk of falls.
Environmental factors include, among others, poor lighting, an inadequate amount, and inaccessible or inconvenient switches, slippery, wet non-slip floors, stairs or sidewalks in poor status, lack of non-slip strips, shoes in poor status or with slippery soles, and household objects that can be tripped over, such as rugs, stools, and electrical cords that can be tripped over.
In relation to patient safety, fall prevention is the sixth international goal. Therefore, the Joint Commission considers patient falls in the hospital setting as a sentinel event, which should be avoided due to the injuries that result from them. In a hospital environment, individuals of any age or physical capability may face the potential of experiencing a fall. This risk can arise from physiological changes resulting from medical conditions, medications, surgical interventions, procedures, or diagnostic tests, which may lead to debilitation or confusion (LeLaurin, 2019).
Strategies to prevent falls proposed by The Joint Commission include:
- Use of standardized assessment to identify risk factors for falls and injury.
- Assessment of individual patient risks that may not have been captured through the tool (for example, using the Morse Fall Scale).
- Interventions tailored to each patient's identified risks.
In addition, the organized and periodic recording and analysis of the institution’s fall incidents are important components of a program focused on falls prevention.
Table 4
Risk Factors and Preventive Measures for Falls
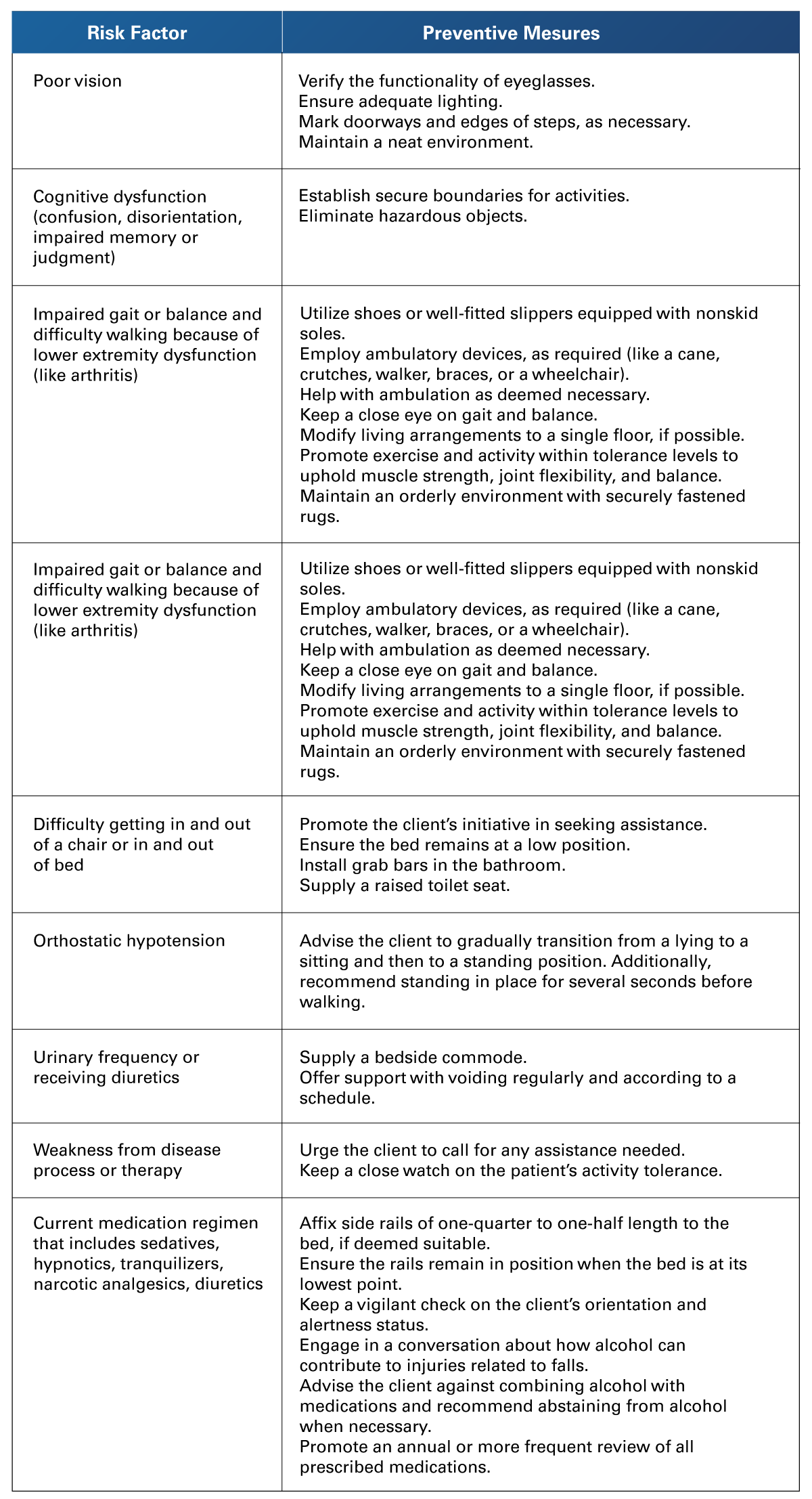 Adapted from Berman et al. (2022). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice. (11th ed.). Pearson Education Limited.
Adapted from Berman et al. (2022). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice. (11th ed.). Pearson Education Limited.
Table 5
Strategies for Fall Prevention
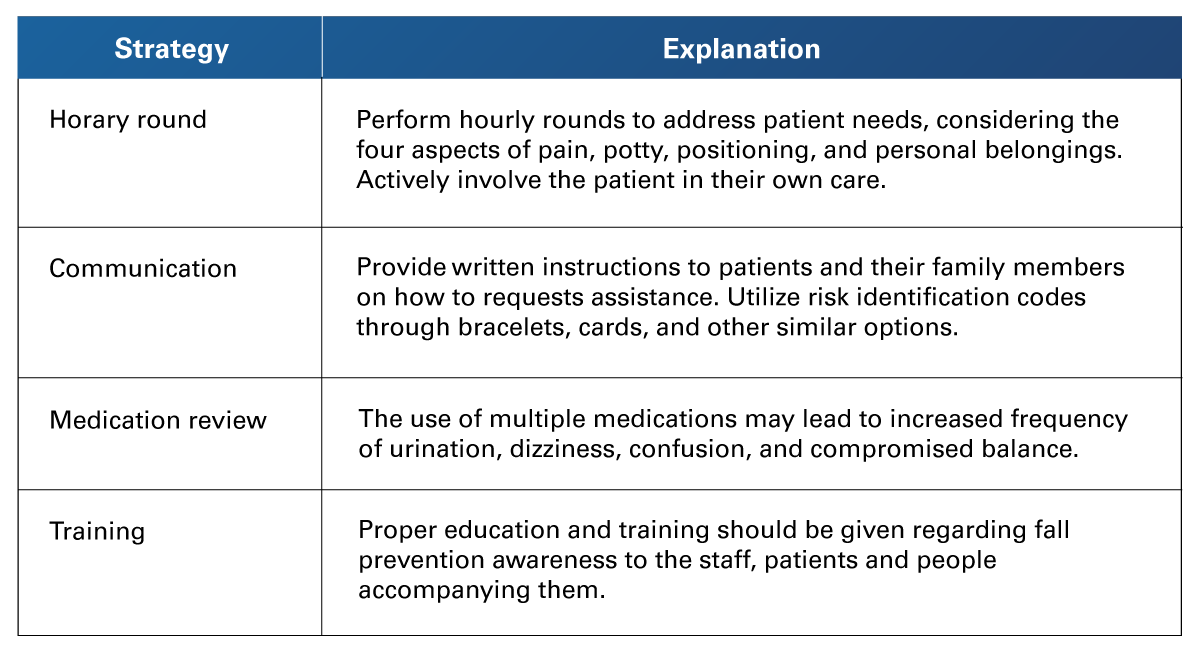 Adapted from Berman et al. (2022). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice. (11th ed.). Pearson Education Limited.
Adapted from Berman et al. (2022). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice. (11th ed.). Pearson Education Limited.
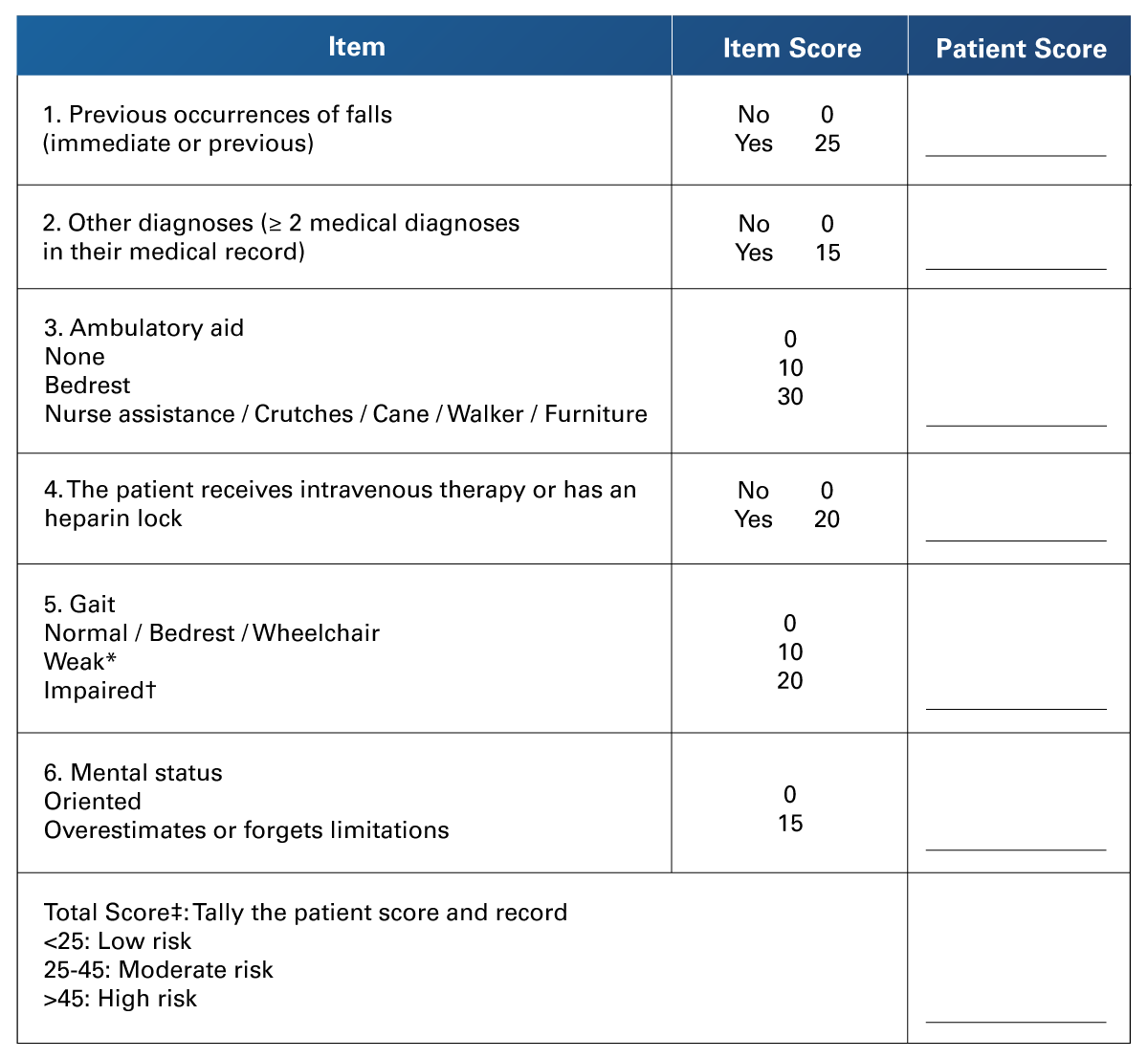
The Morse Fall scale is designed for pinpointing risk factors associated with falls in hospitalized individuals. It is an option to be used by nursing staff. While the overall score can be utilized for forecasting potential falls, the primary emphasis lies in the identification of risk factors through the scale, enabling the development of targeted care plans to address these specific risks. It is suggested to be used alongside clinical assessment and a review of the patient’s medications. Institutions are encouraged to adapt this scale to the risk factors more common to their patient population. When possible, this evaluation should be digitalized and be integrated on a patient’s electronic health record.
Table 6
Morse Fall Scale for Identifying Fall Risk Factors
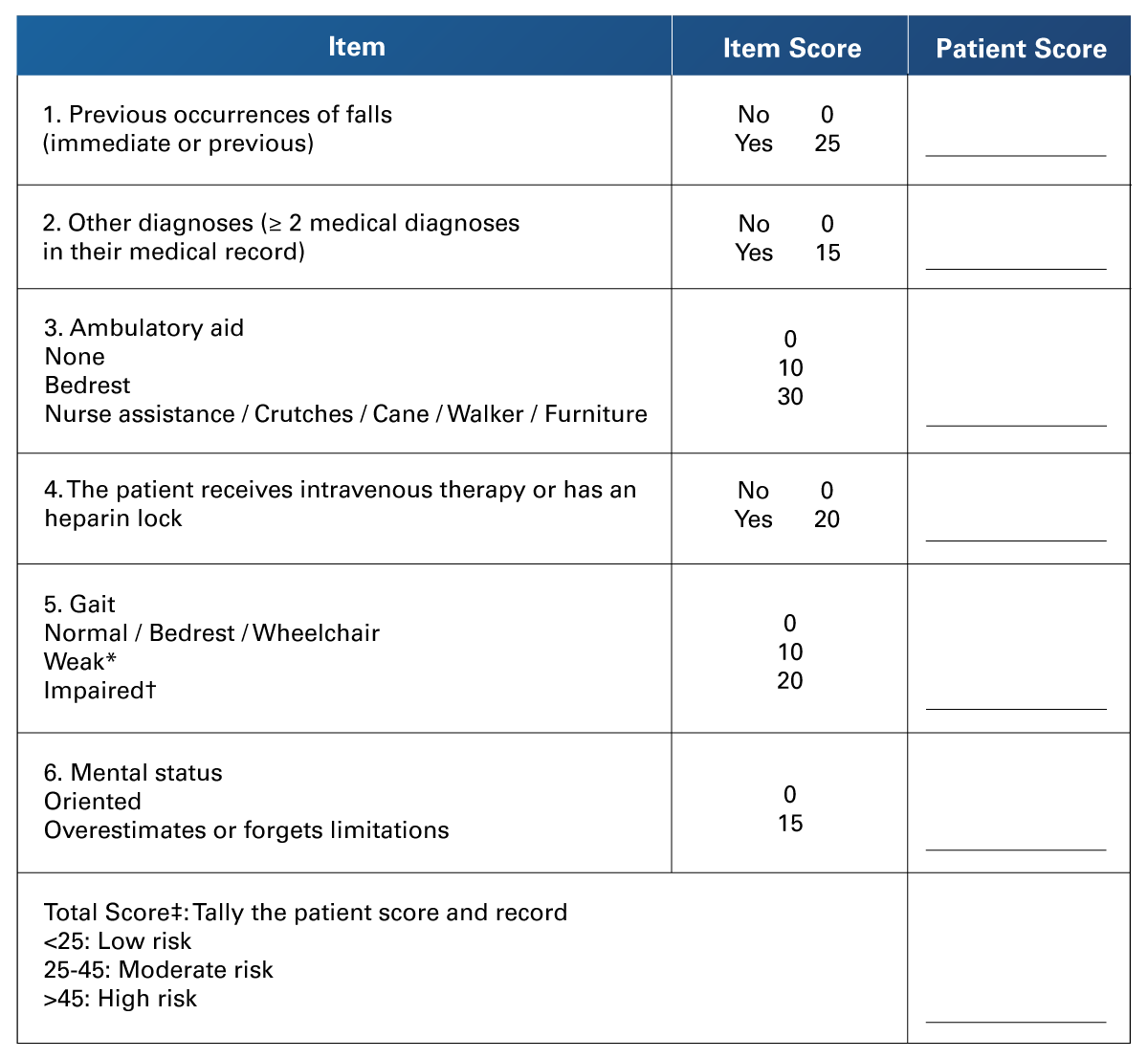
- Weak gait: the patient presents shorts steps and may even shuffle. Even when stooping, they are able to lift their head when walking. Seeking support from furniture is expected, but only with a slight touch, mostly for reassurance.
- Impaired gait: the patient presents short steps with shuffle. They might have a hard time rising from a sitting position. Their heads are mostly down. Their balance is considerably affected. When walking, they need to support on furniture, another person or walking aid.
- Morse noted that the proper cut-points to establish risk should be stated by each particular institution, based on the risk of their patient profile.
Adapted from Bagui et al. (2019). Selecting the Optimal Morse Falls Scale Cut-Off Point for Patient Fall Risk. Health 11(07). https://doi.org/10.4236/health.2019.117074
4.3 Risky Injection Practices
 Parenteral administration by injection is an invasive procedure that must be performed with aseptic techniques because of the risk of infection that can result from needle insertion. The action of a parenterally administered drug is achieved if administered with proper technique. The effect develops depending on the rate at which it is administered and the rate of absorption (Potter et al., 2021).
Parenteral administration by injection is an invasive procedure that must be performed with aseptic techniques because of the risk of infection that can result from needle insertion. The action of a parenterally administered drug is achieved if administered with proper technique. The effect develops depending on the rate at which it is administered and the rate of absorption (Potter et al., 2021).
Safe injection practices are covered in the CDC Standard Precautions used to protect patients and health care personnel. A secure injection is one that does not cause harm to the patient, avoids subjecting the provider to unnecessary risks, and does not produce waste that poses a hazard to the community. (Center for Disease Control and Prevision, 2023).
Table 7
Recommended Practices
 Adapted from Center for Disease Control and Prevision. (2023).
Adapted from Center for Disease Control and Prevision. (2023).
Preventing Injury from Injections and Sharps in Non-U.S. General Healthcare Settings.
https://www.cdc.gov/vhf/ebola/clinicians/non-us-healthcare-settings/safe-injection.html
 These are some of the main events that affect the patients’ evolution and that are a reference to the quality of care provided by the nursing staff. Due to the prevention of pressure sores, falls, and the administration of risk-free injections, nursing staff are the ones who carry out the main preventive measures. It is also true that the patients’ conditions may predispose the development of complications; however, the timely detection of risk factors by the nursing staff is crucial to act in a timely manner and limit the damages. Therefore, it is important to keep in mind these concepts, both for quality daily practice and for the NCLEX accreditation.
These are some of the main events that affect the patients’ evolution and that are a reference to the quality of care provided by the nursing staff. Due to the prevention of pressure sores, falls, and the administration of risk-free injections, nursing staff are the ones who carry out the main preventive measures. It is also true that the patients’ conditions may predispose the development of complications; however, the timely detection of risk factors by the nursing staff is crucial to act in a timely manner and limit the damages. Therefore, it is important to keep in mind these concepts, both for quality daily practice and for the NCLEX accreditation.
- Bagui, S., Long, T., & Bagui, S. (2019). Selecting the Optimal Morse Falls Scale Cut-Off Point for Patient Fall Risk. Health, 11(07), 924. https://doi.org/10.4236/health.2019.117074
- Berman, A., Snyder, S., & Frandsen, G. (2022). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice. (11th ed.). Pearson Education Limited.
- Center for Disease Control and Prevision. (2023, March 24). Preventing Injury from Injections and Sharps in Non-U.S. General Healthcare Settings. https://www.cdc.gov/vhf/ebola/clinicians/non-us-healthcare-settings/safe-injection.html
- LeLaurin, J. H., & Shorr, R. I. (2019). Preventing Falls in Hospitalized Patients: State of the Science. Clinics in Geriatric Medicine, 35(2), 273-283. https://doi.org/10.1016/j.cger.2019.01.007
- Potter, P., Perry, A., Stockert, P., & Hall, A. (2021). Fundamentals of Nursing. (10th ed.). Elsevier.
- World Health Organization. (2020, July 20). Quality Health Services. https://www.who.int/news-room/fact-sheets/detail/quality-health-services
- World Health Organization. (2023, September 11). Patient Safety. https://www.who.int/news-room/fact-sheets/detail/patient-safety
The following links do not belong to Tecmilenio University, when accessing to them, you must accept their terms and conditions.
Readings
- Alshammari, S. M. K., Aldabbagh, H. A., Al Anazi, G. H., Bukhari, A. M., Al Sayed Mahmoud, M., & Mostafa, W. S. E. M. (2023, August 28). Establishing Standardized Nursing Quality Sensitive Indicators. Open Journal of Nursing, 13, 551-582. https://www.scirp.org/pdf/ojn_2023082510453283.pdf
Videos
- World Health Organization. (2017, July 14). Making Injections Safe, We All Have a Part to Play [Video]. https://www.who.int/teams/integrated-health-services/infection-prevention-control/injection-safety#
La obra presentada es propiedad de ENSEÑANZA E INVESTIGACIÓN SUPERIOR A.C. (UNIVERSIDAD TECMILENIO), protegida por la Ley Federal de Derecho de Autor; la alteración o deformación de una obra, así como su reproducción, exhibición o ejecución pública sin el consentimiento de su autor y titular de los derechos correspondientes es constitutivo de un delito tipificado en la Ley Federal de Derechos de Autor, así como en las Leyes Internacionales de Derecho de Autor.
El uso de imágenes, fragmentos de videos, fragmentos de eventos culturales, programas y demás material que sea objeto de protección de los derechos de autor, es exclusivamente para fines educativos e informativos, y cualquier uso distinto como el lucro, reproducción, edición o modificación, será perseguido y sancionado por UNIVERSIDAD TECMILENIO.
Queda prohibido copiar, reproducir, distribuir, publicar, transmitir, difundir, o en cualquier modo explotar cualquier parte de esta obra sin la autorización previa por escrito de UNIVERSIDAD TECMILENIO. Sin embargo, usted podrá bajar material a su computadora personal para uso exclusivamente personal o educacional y no comercial limitado a una copia por página. No se podrá remover o alterar de la copia ninguna leyenda de Derechos de Autor o la que manifieste la autoría del material.