Psychological Adaptation / 06
Make sure to:
- Understand the concept of mental health.
- Differentiate between various classifications of mental illness.
- Understand the historical evolution of mental health and its relationship with nursing.
 Imagine a person with a broken leg that is being asked to constantly run up and down the stairs to fetch things. How considerate does this situation seem? The person is going through a condition that limits their ability to properly function. For a broken leg, the impairment is visible and evident to others. Some illnesses affect the mind and are disadvantageous because they are not visible to others, that can be just as limiting. The quality of performance at daily life activities is very different in people with proper mental health compared to those without.
Imagine a person with a broken leg that is being asked to constantly run up and down the stairs to fetch things. How considerate does this situation seem? The person is going through a condition that limits their ability to properly function. For a broken leg, the impairment is visible and evident to others. Some illnesses affect the mind and are disadvantageous because they are not visible to others, that can be just as limiting. The quality of performance at daily life activities is very different in people with proper mental health compared to those without.
Mental health is a fundamental part of well-being that supports individual and collective abilities to make decisions, establish relationships and shape the world in which one lives.
Studies conducted in 2019 revealed that approximately 1 in 8 individuals worldwide suffer from a mental disorder (World Health Organization, 2022a). It has also been noted that since the 2020 pandemic, these conditions have increased considerably.
Throughout life, various psychological and biological factors can make people more vulnerable to mental health conditions.
Nursing interventions for the specific care of patients with these pathologies focus on promotion and prevention. For nurses, it's also crucial to have the ability to identify the social, individual, and structural determinants of mental health. This helps reduce risks, increase resilience, and foster environments conducive to sustaining good mental health.
1.1 Concept of Mental Health
 The World Health Organization (2022b) defines mental health as a state of psychological well-being, enabling individuals to handle life's stress, nurture skills, function in learning and work, and contribute positively to their community. Mental health is a fundamental part of a person’s health and well-being, providing the ability to make decisions, establish positive connections with others and interact with our environment. Also, it is considered a basic human right and a central factor in the proper development of both the individual and the community.
The World Health Organization (2022b) defines mental health as a state of psychological well-being, enabling individuals to handle life's stress, nurture skills, function in learning and work, and contribute positively to their community. Mental health is a fundamental part of a person’s health and well-being, providing the ability to make decisions, establish positive connections with others and interact with our environment. Also, it is considered a basic human right and a central factor in the proper development of both the individual and the community.
Practically speaking, since it is a fundamental facet of personal health, mental health is a basic human right, pivotal for both individual and societal development.
1.2 Health Concepts – Mental Illness
Determinants of Mental Health
 There are various individual factors that can make people vulnerable to mental health conditions. These include both psychological and biological factors, such as emotional abilities, history of substance abuse and genetics.
There are various individual factors that can make people vulnerable to mental health conditions. These include both psychological and biological factors, such as emotional abilities, history of substance abuse and genetics.
Exposure to certain external factors may also increase the risk of suffering from mental health conditions. Examples of these would include unfavorable social, economic, geopolitical and environmental circumstances, like violence, poverty or inequality.
Risk factors predisposing individuals to mental illnesses can arise at any life stage. Those manifesting during sensitive developmental phases, like childhood, carry pronounced detriment. Within the community, global threats increase the risk for entire populations. At this level, some examples of risks would include economic recessions, disease outbreaks and humanitarian emergencies (World Health Organization, 2022b). Below is a table highlighting the protective and risk factors of mental health across different societal levels:
Table 1
Social and Environmental Determinants of Mental Health
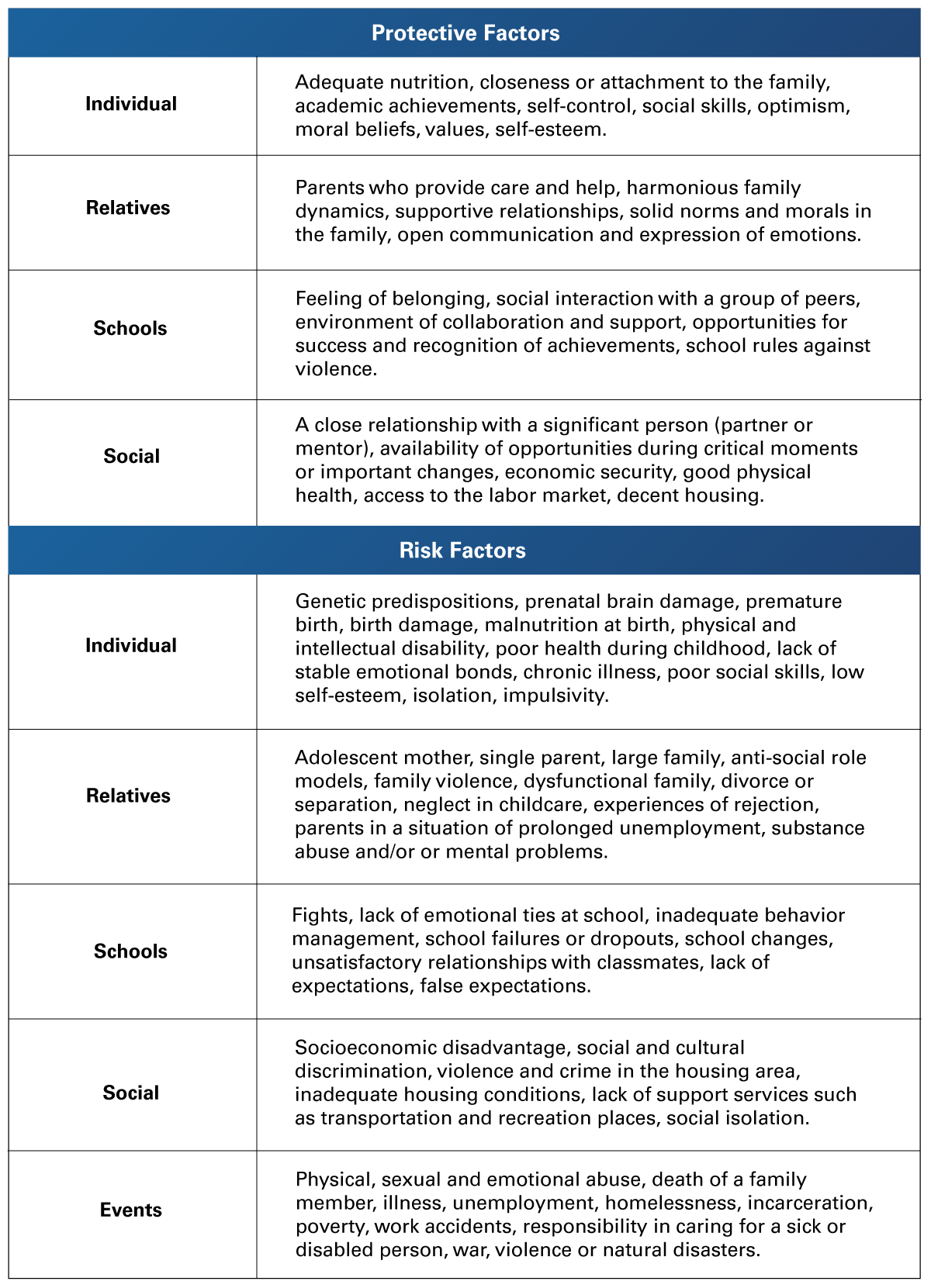 Adapted from Rentería, M. (2018). Mental Health in Mexico. INCyTU, 7. https://www.foroconsultivo.org.mx/INCyTU/documentos/Completa/INCYTU_18-007.pdf
Adapted from Rentería, M. (2018). Mental Health in Mexico. INCyTU, 7. https://www.foroconsultivo.org.mx/INCyTU/documentos/Completa/INCYTU_18-007.pdf
Mental Illnesses/Disorders:
 A mental disorder involves a clinically significant alteration of an individual's cognitive abilities, behavior or emotion regulation. It is generally associated with distress or functional disability in other important areas.
A mental disorder involves a clinically significant alteration of an individual's cognitive abilities, behavior or emotion regulation. It is generally associated with distress or functional disability in other important areas.
Some other references establish that mental illnesses or disorders are the product of sustained emotional, behavioral, and/or cognitive alterations. In these conditions, the basic psychological processes such as motivation, emotion, consciousness, cognition, perception, behavior, sensation, language, and learning are affected. These alterations provide difficulty for the person to adapt to their social and cultural environment, which may produce subjective discomfort (Chatmon, 2020).
Studies carried out globally estimate that in 2016, between 450 and 500 million people had some mental disorder. The World Health Organization estimates that more than 300 million suffer from depression, 60 million from bipolar disorder and almost 21 million suffer schizophrenia (World Health Organization, 2022a). In addition, almost a million people commit suicide each year, which represents more deaths than those generated by war conflicts and natural disasters combined.
Another statistical report carried out by the same organization concluded that in 2019, the world prevalence of mental disorders was 12.5% (World Health Organization, 2022b). After the COVID-19 pandemic in 2020, the initial estimates were that there was an increase of up to 28% in conditions such as anxiety and severe depressive disorders.
Mental health conditions represent up to 15% of the global economic burden of disease. Also, 33% of the average years lived with disability are attributable to mental disorders. It is estimated that by 2030, depression will be the second cause of decreased years of healthy life worldwide.
Table 2
Most Prevalent Mental Illnesses/Disorders
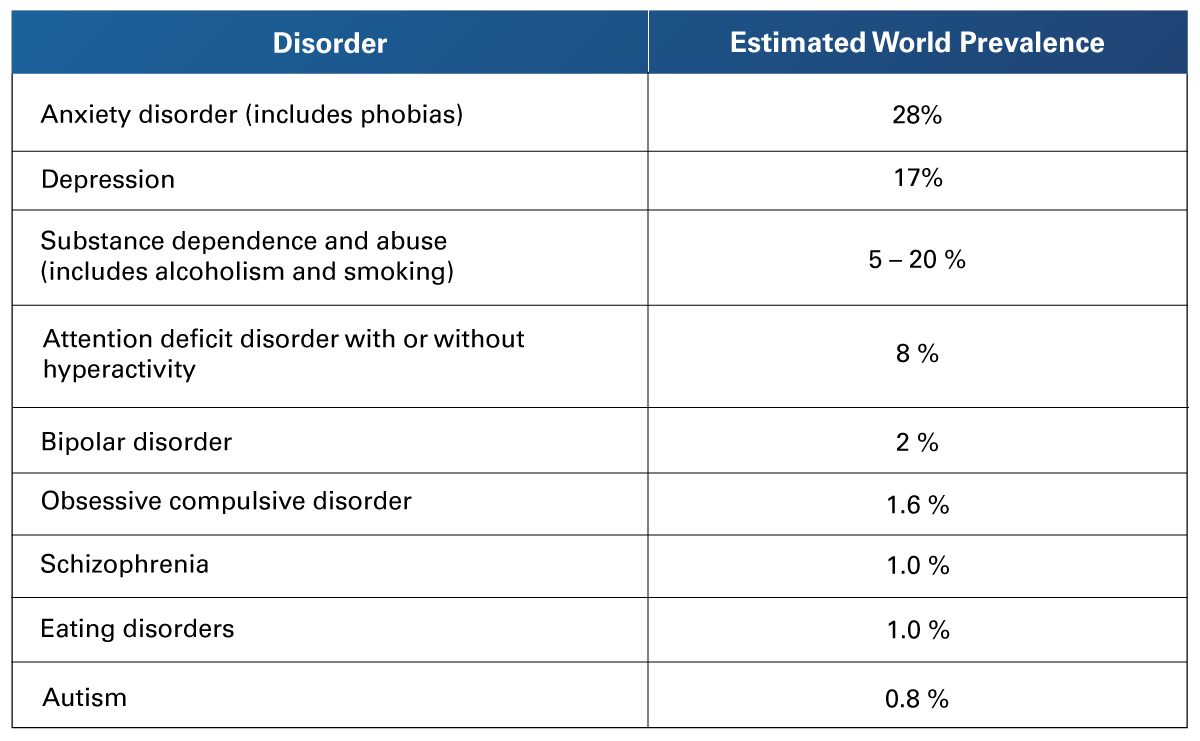 Adapted from Rentería, M. (2018). Mental Health in Mexico. INCyTU, 7. https://www.foroconsultivo.org.mx/INCyTU/documentos/Completa/INCYTU_18-007.pdf
Adapted from Rentería, M. (2018). Mental Health in Mexico. INCyTU, 7. https://www.foroconsultivo.org.mx/INCyTU/documentos/Completa/INCYTU_18-007.pdf
The WHO recommendations
The member states of the WHO have committed to putting into practice the Comprehensive Action Plan on Mental Health 2013-2030, which main objective is improving mental health through more effective health policies that are characterized by the provision of health services. It also suggests more effective, complete care, integrated and adapted to needs in a community framework, as well as the application of promotion and prevention strategies.
The World Mental Health Report: Transforming Mental Health for All, published by the World Health Organization (2022b), invites all countries to accelerate the implementation of action plans, stressing that significant progress can be achieved globally in improving the mental health of their population by focusing on the following transformation activities:
- Increasing the value and importance given to mental health by individuals, communities, and governments, making all sectors commit to mental health and making comprehensive investments that favor its development.
- Acting on the economic, social and physical characteristics of family, school, work and community environments to protect mental health and prevent mental illnesses.
- Strengthening mental healthcare so that the entire range of needs in this area is covered by a community network that has available affordable and quality support services.
1.3 Historical Evolution of Mental Health
 During the time of the Second World War, it became evident that the patients admitted to psychiatric hospitals lived in desolate situations and that many therapies applied were ineffective. The areas of opportunity were identified, and a goal was set to provide quality care to these patients, considering their human rights and their dignity. Treatments needed to be updated too, to assure that the illnesses were being managed effectively.
During the time of the Second World War, it became evident that the patients admitted to psychiatric hospitals lived in desolate situations and that many therapies applied were ineffective. The areas of opportunity were identified, and a goal was set to provide quality care to these patients, considering their human rights and their dignity. Treatments needed to be updated too, to assure that the illnesses were being managed effectively.
In the therapeutic and organizational strategy, a triple displacement of power and therapeutic benefit occurs, from the hospital to the territory, from the psychiatrist to the multidisciplinary team and from the sick subject to the community of which he or she is a part. This brought about a new culture in the field, combining psychiatric, psychological and social aspects. The clinical practice now focused on the individual and the biological reasonings behind the conditions. The new model required not only new practices in the daily activities carried out by health professionals but also the plans and organization of the public system.
In 1908, Cliffor Beers, a former patient admitted to several psychiatric hospitals, published a book titled The Mind That Found Itself that shifted public opinion and aided in the promotion of the Mental Hygiene League.
The Second World War provided the scenario for the administrative and clinical reorganization of psychological care. The lack of personnel in the psychiatric institutions gave rise to two increasingly effective methods of care in treatment: institutional coexistence and psychotherapy. The first removed the stigma surrounding mental conditions as different from other physical illnesses, and the second provided a new approach to the treatment of these conditions.
French Institutional and the English Therapeutic Community
The Saint-Alban psychiatric hospital was stablished in what was once a rural asylum, and it was the birthplace of the French institutional psychotherapy model of care. This model applies the hypothesis that it is not the walls of a hospital that make an asylum, it is the caregivers and patients who live there. Therefore, therapy must encompass the entire hospital, the staff and the patients; it is the whole institution that must be treated.
After the liberation, institutional psychotherapy became the theoretical foundation of French psychiatry. This consolidated the presence of psychoanalysis together with the work of the community. This is how the Saint-Alban Hospital became a meeting and training place for psychiatrists who would become the protagonists of the reformation of mental health care in France.
In 1943, at the Northfield Hospital of England, a new organization model was implemented, which came to be known as the therapeutic community. The patients at Northfield were mainly soldiers with mental disorders and the new model proposed that they organize a hospital government were doctors, patients and auxiliary personnel were all in charge of activities and responsibilities in a non-hierarchical way.
In 1963, President John F. Kennedy presented to the United States Congress the law that promulgates the creation of community mental health centers for the prevention or diagnosis of mental illness, the assistance and treatment of the mentally ill, and the rehabilitation of those people, a fact that is established as the launch of community mental health in the United States. This initiative proposed the creation of community mental health centers throughout the nation, in response to the complaints of mentally ill patients admitted to psychiatric hospitals and the lack of extra-hospital public assistance. This speech was the beginning of a revolution in North American psychiatry in terms of the prevention, treatment and rehabilitation of the mentally ill.
Mental Health in Latin America
The psychiatric reform projects appear in Latin America after the Caracas Conference of 1954, when the Pan American Health Organization discussed the matters of mental health, asylums, and their necessary deinstitutionalization. The principles approved in Caracas had a great impact in Latin American countries, modifying legislation to guarantee greater protection for people with psychological problems and approving health plans that attempted to introduce changes in mental healthcare.
Although the conclusion of the conference was signed by the health ministers of the countries of Latin America and the Caribbean, in Brazil, Chile and very recently in Peru, national mental health plans have been developed in accordance with these principles. In these circumstances, community mental health becomes a resource for the poor, poorly financed and for those who are outside of any health systems.
Carrying out a historical summary after what has already been reviewed, it is hard to deny the great achievements of the psychiatric reform process. The advantages of deinstitutionalization and the creation of the community mental health model are evident. There are still many challenges being faced in all countries, especially in those where the model of the isolated psychiatric houses persists. A positive development is the loss of the taboo surrounding mental conditions. There is greater social awareness of the neglect and poor actions of governments regarding mental health care. In the field of health management, the closure of asylums and the creation of services in the community are increasingly seen as an optimization of the resources. Whether this is done for the preservation of public resources, or for the profit of a private management, there are many nuances to these markets (Desviat, 2020).
 As mentioned by the WHO (2022a), “health is a state of complete physical, mental and social well-being, and not only the absence of conditions or diseases,” which is why the study of mental health, and its historical antecedents are of great importance. Understanding the pathological phenomena that impact such a large segment of the global population has led to increases in diagnosis rates and a heightened overall awareness. Therefore, it is important for any nurse to identify that the care of these patients must be comprehensive. They may need guidance with educational programs, employment opportunities, housing options, and participation in other meaningful activities.
As mentioned by the WHO (2022a), “health is a state of complete physical, mental and social well-being, and not only the absence of conditions or diseases,” which is why the study of mental health, and its historical antecedents are of great importance. Understanding the pathological phenomena that impact such a large segment of the global population has led to increases in diagnosis rates and a heightened overall awareness. Therefore, it is important for any nurse to identify that the care of these patients must be comprehensive. They may need guidance with educational programs, employment opportunities, housing options, and participation in other meaningful activities.
It has been identified that the response of the health systems around the world has not been adequate to the people living with mental disorders, mainly because of a lack of resources. The necessity for treatments and their availability is not the same in the different regions and countries. The quality of these services is not equal either. It has been cited that only 29% of people with psychosis and only 33% of people with depression have access to proper mental health care, as part of a formal health system (World Health Organization, 2022b).
Going back to the initial example of the person with a broken leg being asked to go up and down the stairs, it is easier now to comprehend how complex the interaction between risk factors and available resources is. Nurses must have the empathy and knowledge to properly treat these patients so they may achieve the best quality of life possible for them.
- Chatmon, B. (2020). Males and Mental Health Stigma. American Journal of Men's Health, 14(4). https://journals.sagepub.com/doi/full/10.1177/1557988320949322
- Desviat, M. (2020). Historical Evolution of Mental Health Care: Essential Milestones in the Construction of the Community Mental Health Discourse. Social Education: Journal of Socio-Educational Intervention. 75(May-August), 17-45. https://www.raco.cat/index.php/EducacioSocial/article/view/367856/466393
- Rentería, M. (2018, January). Mental Health in Mexico. INCyTU, 7. https://www.foroconsultivo.org.mx/INCyTU/documentos/Completa/INCYTU_18-007.pdf
- World Health Organization. (2022a, June 8). Mental Disorders. https://www.who.int/news-room/fact-sheets/detail/mental-disorders
- World Health Organization. (2022b, June 17). Mental Health: Strengthening our Response. https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response
The following links do not belong to Tecmilenio University, when accessing to them, you must accept their terms and conditions.
Videos
- Cambridge University. (2022, January 21). Podcast: Mental Health and Young People [Video]. YouTube. https://youtu.be/01wcrrAYrpM?si=mZQol--DMGUiQNMk
- TEDx Talks. (2023, January 20). The Power of Struggling with Mental Illness | Piper Garner | TEDxOshkosh [Video]. YouTube. https://youtu.be/YD0fsTfPblg?si=bJZqTrNrEDt6uTba
Readings
- Smith, Y. (2019). Mental Health Nursing. News-Medical Life Sciences. https://www.news-medical.net/health/Mental-Health-Nursing.aspx
La obra presentada es propiedad de ENSEÑANZA E INVESTIGACIÓN SUPERIOR A.C. (UNIVERSIDAD TECMILENIO), protegida por la Ley Federal de Derecho de Autor; la alteración o deformación de una obra, así como su reproducción, exhibición o ejecución pública sin el consentimiento de su autor y titular de los derechos correspondientes es constitutivo de un delito tipificado en la Ley Federal de Derechos de Autor, así como en las Leyes Internacionales de Derecho de Autor.
El uso de imágenes, fragmentos de videos, fragmentos de eventos culturales, programas y demás material que sea objeto de protección de los derechos de autor, es exclusivamente para fines educativos e informativos, y cualquier uso distinto como el lucro, reproducción, edición o modificación, será perseguido y sancionado por UNIVERSIDAD TECMILENIO.
Queda prohibido copiar, reproducir, distribuir, publicar, transmitir, difundir, o en cualquier modo explotar cualquier parte de esta obra sin la autorización previa por escrito de UNIVERSIDAD TECMILENIO. Sin embargo, usted podrá bajar material a su computadora personal para uso exclusivamente personal o educacional y no comercial limitado a una copia por página. No se podrá remover o alterar de la copia ninguna leyenda de Derechos de Autor o la que manifieste la autoría del material.