Basic Care and Comfort / 03
Make sure to:
- Remember necessary knowledge to determine clients’ needs for daily living activities.
- Determine techniques and methods to assess clients’ needs for daily living activities.
- Employ evidence-based interventions to assist the client in daily living activities.
 Dorothea Orem’s theory emphasizes that nursing care should be provided either fully or partially, depending on the client’s inability to perform tasks independently (Tanaka, 2022). Assessing the client's daily living needs represents the most fundamental level of nursing assistance aimed at promoting health, preventing illness, assisting in rehabilitation, helping with palliative care, and even providing postmortem care. Subsequently, the nurse will need to recollect essential, evidence-based information to deliver nursing care for the client's daily activities of living.
Dorothea Orem’s theory emphasizes that nursing care should be provided either fully or partially, depending on the client’s inability to perform tasks independently (Tanaka, 2022). Assessing the client's daily living needs represents the most fundamental level of nursing assistance aimed at promoting health, preventing illness, assisting in rehabilitation, helping with palliative care, and even providing postmortem care. Subsequently, the nurse will need to recollect essential, evidence-based information to deliver nursing care for the client's daily activities of living.
1.1 Assessment of Daily Living Activities Performance and Personal Hygiene
 Since people are so different, numerous factors come into play in hygiene habits and routines. These factors might be environmental factors (such as temperature, water availability, water quality, and privacy), economic factors (such as financial constraints affecting basic hygiene necessities like soap, toothpaste, and shampoo), cultural factors (including family routines, traditions, religion, and beliefs), and personal factors (like age, life stage, education, religious beliefs, knowledge level, cognitive ability, energy level, health status, and housing situation), among others. Consequently, care must be customized to accommodate these individual characteristics.
Since people are so different, numerous factors come into play in hygiene habits and routines. These factors might be environmental factors (such as temperature, water availability, water quality, and privacy), economic factors (such as financial constraints affecting basic hygiene necessities like soap, toothpaste, and shampoo), cultural factors (including family routines, traditions, religion, and beliefs), and personal factors (like age, life stage, education, religious beliefs, knowledge level, cognitive ability, energy level, health status, and housing situation), among others. Consequently, care must be customized to accommodate these individual characteristics.
Nurses must assess a client’s ability to perform a range of activities, including personal hygiene, mobility, ambulation, toileting, personal care, grooming, dressing, and eating. The assessment of daily living activities performance includes observations related to the ability to move, tolerance for changes, and the use of medical devices.
Assessing the Cognitive Level of Functioning during the Mental Status Examination involves evaluating judgment, orientation, attention span, recent memory, remote memory, thought processes, and perceptions (Silvestri & Silvestri, 2022). This information is crucial for determining the level of independence or dependence on each activity and providing the necessary total or partial support as required (Nasiri et al., 2022).
- Bathing, Showering, and Washing
Assessing the client's ability to shower involves gathering information on their ability to move, maintain balance, demonstrate muscle strength, exhibit flexibility, cope with sensory-perceptive changes, use medical devices, and assess the risk of falls. It also involves evaluating the frequency of grooming and the effectiveness of grooming techniques. Three distinct bathing techniques are available for clients:
A. Bathing in a shower or bathtub. This is a technique suitable for clients who have total or partial mobility. If mobility is partial or if there are sensory-perceptive alterations that cause a risk of falling, it becomes necessary to install handrails, bathroom chairs, and emergency alert mechanisms. The decision to accompany the patient during the shower should be evaluated.
B. Partial bed bathing. This is a technique designed for clients who can independently perform hygiene activities or require partial support. There is a need to implement safety measures, such as bed rails, to prevent falls.
C. Complete bed bathing. This is a technique offered to clients who are unable to independently perform hygiene activities. The necessity of implementing safety measures, such as bed rails, to prevent falls should be evaluated. In cases where total support is needed, bath time must be used as an opportunity to assess skin integrity.
Assessment of skin integrity includes aspects such as color, texture, thickness, turgor, temperature, odors, lesions, dryness, scaling, and cracking (Silvestri & Silvestri, 2022). Additionally, it is important not to overlook inquiries about allergies.
- Hair Care
Hair grooming can be performed in any type of bathroom. While grooming or brushing, one can assess factors such as hair implantation strength, hair quality, and the presence of conditions like alopecia, pediculosis, or dandruff. In cases where clients face mobility problems, it is important to ensure that the hair is completely dried to prevent moisture in the bed.
- Mouth and Oral Care
Teeth cleaning should be performed after every meal, preferably before bedtime. Tooth brushing can be supplemented with mouthwash and dental floss. It is important to assess for the presence of cavities, tooth loss, compromised integrity of the oral mucosa, or infections. Mobile dentures should be removed for brushing and stored in a protective device to shield them from dust and other particles when not in the oral cavity. It is worth noting that chlorhexidine gluconate can reduce the risk of ventilator-associated pneumonia.
- Shaving
Beard and body hair, whether in the armpits or on the legs, are integral components of an individual’s personal image. Clients should be encouraged to maintain clean and well-groomed body hair. It is essential to assess for the presence of pediculosis or any wounds caused by shaving that might require attention. If a client requires assistance with shaving, the proper technique involves the use of warm water and soap or shaving cream to minimize the risk of irritation.
- Nail Care
Toenails should be cleaned daily during bathing. As for fingernails, they should not be cleaned in the bathroom but washing the hands thoroughly. It is important to assess their color, quality, cleanliness, length, and check for the presence of ingrown nails, fungus, or infections. In the case of patients with diabetes, special attention should be given to preventing infections, and priority should be given to treating any wounds.
- Foot Care
Feet should be cleaned daily during bathing and should then be kept dry, well-ventilated, and protected with suitable footwear. It is important to assess for the presence of wounds, calluses, corns, plantar warts, tinea pedis, paronychia, or any other conditions that might require attention, especially in patients with diabetes.
- Toileting
Some patients frequently experience difficulties that compel them to rush to the bathroom. This can lead to discomfort for the client and an elevated risk of infection, or skin breakdown. The urgency to use the bathroom might arise from movement impairments, incontinence problems, dementia, or interactions with specific medications.
According to the University of Nebraska Medical Center (n.d.), some of the nursing interventions are:
- Assess the level of dependence on bathroom visits.
- Establish communication channels with the patient at all times, including during emergencies.
- Consult with the patient regarding their preferences and the availability of medical equipment that can assist such as diapers, portable toilets, commodes, or urinals.
- Educate the family and health personnel on safely transferring the patient from the bed to the bathroom and vice versa.
- Provide patient education on exercises aimed at strengthening the sphincters.
- Establish a schedule based on the patient's daily activities, including waking up and post-meals routines.
Ensure to assess the risk of falls and the condition of the skin following each toileting episode, whether for defecation or urination, to identify and prevent injuries and urinary tract infections.
- Perineal Care
Perineal cleansing is performed during bathing to prevent unpleasant odors and infections. It is essential to assess the skin’s integrity, as well as check for secretions, odors, or signs of infections. In patients with diaphoresis, fecal or urinary incontinence, or those with devices such as a urinary catheter or indwelling urinary catheters, the frequency of grooming might need to be increased.
- Dressing
Dressing is a daily routine that can pose challenges for older adults, individuals with mental health issues, or those with mobility impairments. It is essential to ensure that the choice of clothing aligns with the person’s environment and condition. For example, a person with total immobility benefits from wearing a gown for ease during daily care activities. In contrast, a pediatric patient requires more insulation due to the risk of losing body heat through convection mechanisms. Similarly, older adults might require extra insulation due to difficulties in maintaining body heat because of their metabolic characteristics. It is crucial to maintain clean clothing that poses no risks to the patient. In cases where the patient undergoes surgery, clothing with low conductivity is preferred, with cotton being a suitable choice.
- Post-mortem Care
 Postmortem care is administered with the same level of respect and compassion extended to living individuals. Nursing interventions include grooming the client's body, removing all devices, tubes, and fixations, and carefully positioning the body while ensuring the eyes and jaw are closed. It is essential not to overlook the need to properly identify the body and cover it completely before transferring it to the morgue.
Postmortem care is administered with the same level of respect and compassion extended to living individuals. Nursing interventions include grooming the client's body, removing all devices, tubes, and fixations, and carefully positioning the body while ensuring the eyes and jaw are closed. It is essential not to overlook the need to properly identify the body and cover it completely before transferring it to the morgue.
1.2 Feeding and Hydration
Preferences, Routines, and Abilities
Food is integral to people’s culture, intricately tied to customs, memories, emotions, routines, beliefs and even religions, making it challenging to modify due to its deep-seated roots. It is essential to perform a detailed evaluation of each person's circumstances to identify their eating preferences and routines, facilitating dietary adjustments that align with these individual characteristics and promote stronger adherence. In addition to culture, external factors such as socioeconomic status, geography, and environmental conditions can also impact one’s diet.
On the other hand, intrinsic factors that can influence one’s diet include age, life stage, sex, pregnancy, social role, occupation, work environment, education, personal beliefs, perceived and desired body image, friendships, psychological state, medications that, when interacting with food, might enhance, inhibit or reduce the intended effects. Additionally, health status, encompassing general pathologies in the gastrointestinal tract, dental condition, oral health, and eating abilities, plays a significant role in dietary choices.
Managing the Client's Nutritional Intake
a) Assessment
Nutrition forms the foundation of all body tissues and organs composition, thus exerting a significant impact on health. The initial assessment of nutritional status begins with the general appearance of the individual. In a cephalocaudal approach, the following aspects are considered in the physical assessment:
- The patient's level of alertness.
- The condition of the skin, which should appear turgid, glossy, and free from dryness.
- Healthy, shiny, and well-maintained hair with no signs of alopecia.
- Deep red color of the tarsal mucosa.
- Hydrated oral mucosa.
- Complete, healthy, and strong teeth.
- A tongue displaying a deep red color.
- Firm gums, without redness.
- Nails without ridges.
- Strong extremities with a good range of motion.
- A skeleton without malformations.
- An erect posture.
- Firm muscles.
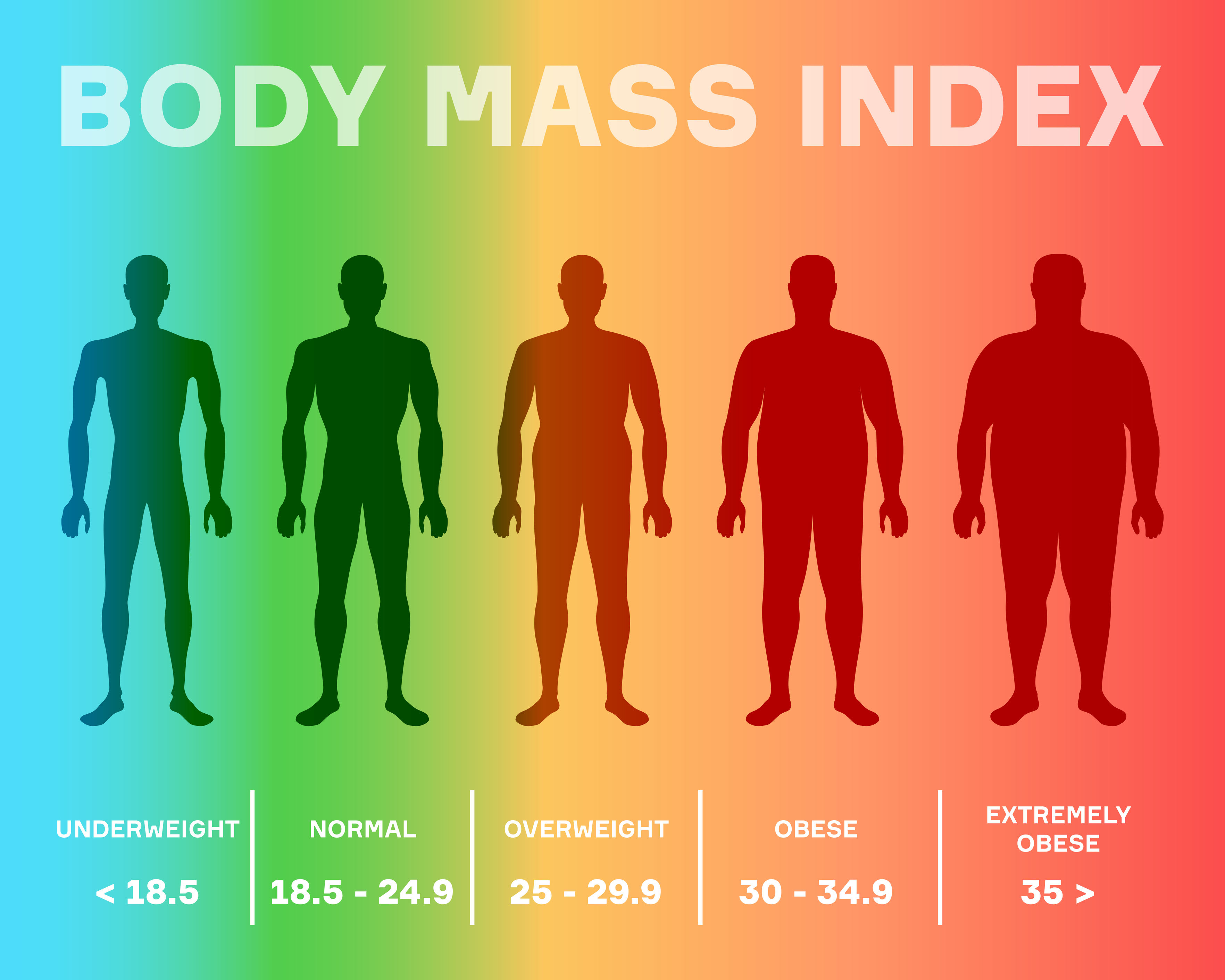
- A healthy weight and normal BMI (Body Mass Index= Weight/Height2). It is important to remember the BMI classification:
- Underweight: BMI < 18.5
- Normal weight: BMI 18.5 - 24.9
- Overweight: BMI 25 - 29.9
- Obesity (Class I): BMI 30 - 34.9
- Obesity (Class II): BMI 35 - 39.9
- Obesity (Class III): BMI ≥ 40
The subjective data that can be obtained from the client includes information about their eating habits and routines over a 24-hour, weekly or monthly period, medication intake, changes in weight or eating patterns, and their perceived and desired body image.
According to Kaplan Nursing (2023) variations influenced by religion or culture may include:
- Orthodox Jewish. They have strong dietary laws, such as never consuming milk at the same meal as meat or at least 6 hours later. Meat is only consumed once a day and must be drained of blood (Kosher). They also abstain from consuming pork, diseased animals, or those who die from natural causes, as well as fish without fins or scales, like oysters, crabs, or lobsters.
- Muslim. They also have strong dietary laws based on the Koran, which prohibited the consumption of fermented food, pork, or alcohol. Meat must be prepared in accordance with Halal guidelines and the humane process of animal slaughter is essential. Additionally, during Ramadan, Muslims have a 30-day period of daylight fasting.
- Puerto Rican. Their meals are typically centered around rice, beans, vegetables, and fruits.
- Hispanic. Meals often feature saturated fats and are based on corn, beans, chili peppers, and vegetables.
- African American. Their diet frequently includes leafy greens, pork, fat, cholesterol, and sodium.
- Native American. Traditional meals are characterized by a wide variety of foods, often prepared by frying.
It is worth mentioning that various dietary preferences exist, including vegetarian diets (excludes red meat, chicken, and seafood but allows dairy products), vegan diets (excludes red meat and all animal products), lacto-vegetarian diets (excludes red meat but allow eggs and dairy products), ovo-vegetarian diets (rely only on eggs as the sole source of animal protein), lacto-ovo vegetarian diets (include eggs and other dairy products), and diets that abstain from red-meat.
Subsequently, the evaluation will include an assessment of family history, including metabolic conditions, diabetes, hypertension, and other relevant factors. Finally, personal pathological history such as surgeries, and pathologies that alter mobility or metabolism.
b) Calculating Requirements
An adult requires an estimated daily intake of between 1,500 and 3,000 kcal. It is essential that the diet is both diverse and of high quality, with adequate quantities of essential nutrients, and well balanced.
The quantity of calories is adjusted based on the individual’s Body Mass Index BMI (BMI=kg/m2) and level of physical activity. Nursing interventions include educating the client on calorie counting and how to create balanced, nutritious meals through food combination. In case of fluids, one lost kilogram is equivalent to losing one liter of fluids and, one kilogram earned is equivalent to earning one liter of fluids according to Kaplan Nursing (2023).
c) Adjusting the Diet
Depending on individual’s health conditions, the diet can be customized in the following ways:
- Full liquid diet. This diet consists solely of fluids with vitamin content; it excludes juices and milk. It is commonly used in short post-operative recovery periods or during acute gastrointestinal pathologies under evaluation.
- Clear liquid diet. This diet includes more substantial but not solid foods like gelatin, juices, or blended fruit. It is frequently prescribed for extended post-operative recovery periods or during gastrointestinal pathologies under evaluation.
- Low-fat, cholesterol-restricted diet. This diet incorporates solid foods such as fruits, vegetables, and lean meat. It is recommended for clients with cardiovascular pathologies, gastrointestinal disorders, or weight problems. These patients may also require education on statins, which are medications used to reduce cholesterol.
- Low calorie diet. This diet provides the minimum calorie intake required based on BMI and is primarily used for weight management.
- Low in sodium diet. A sodium-free diet or low-sodium diet is recommended for clients with conditions like cardiovascular, hepatic, renal, or hormonal diseases.
- Low in sugar diet. This diet is either sugar-free or low in sugar and is recommended for clients with diabetes.
- High-roughage, high-fiber diet. Recommended for those needing to increase natural fiber intake or fiber supplements to promote regular bowel movements.
- High-protein diet. Recommended for clients with burns, infection, and hyperthyroidism (Kaplan Nursing, 2023).
It is essential to adapt the diet to meet specific requirements depending on medical diagnoses such as hepatic, renal, cardiac, and gastrointestinal, and other conditions.
d) Provide Client Nutrition through Continuous or Intermittent Tube Feedings
Some medical conditions cause the inability to use the gastrointestinal route, such as major abdominal surgeries, gastrointestinal paralysis, or gastrointestinal obstruction. An alternative feeding method involves administrating a liquid diet through a tube placed on the stomach, duodenum, or proximal jejunum. Nurses must be attentive to the unique care requirements associated with each method of feeding.
Table 1
Type of Feedings
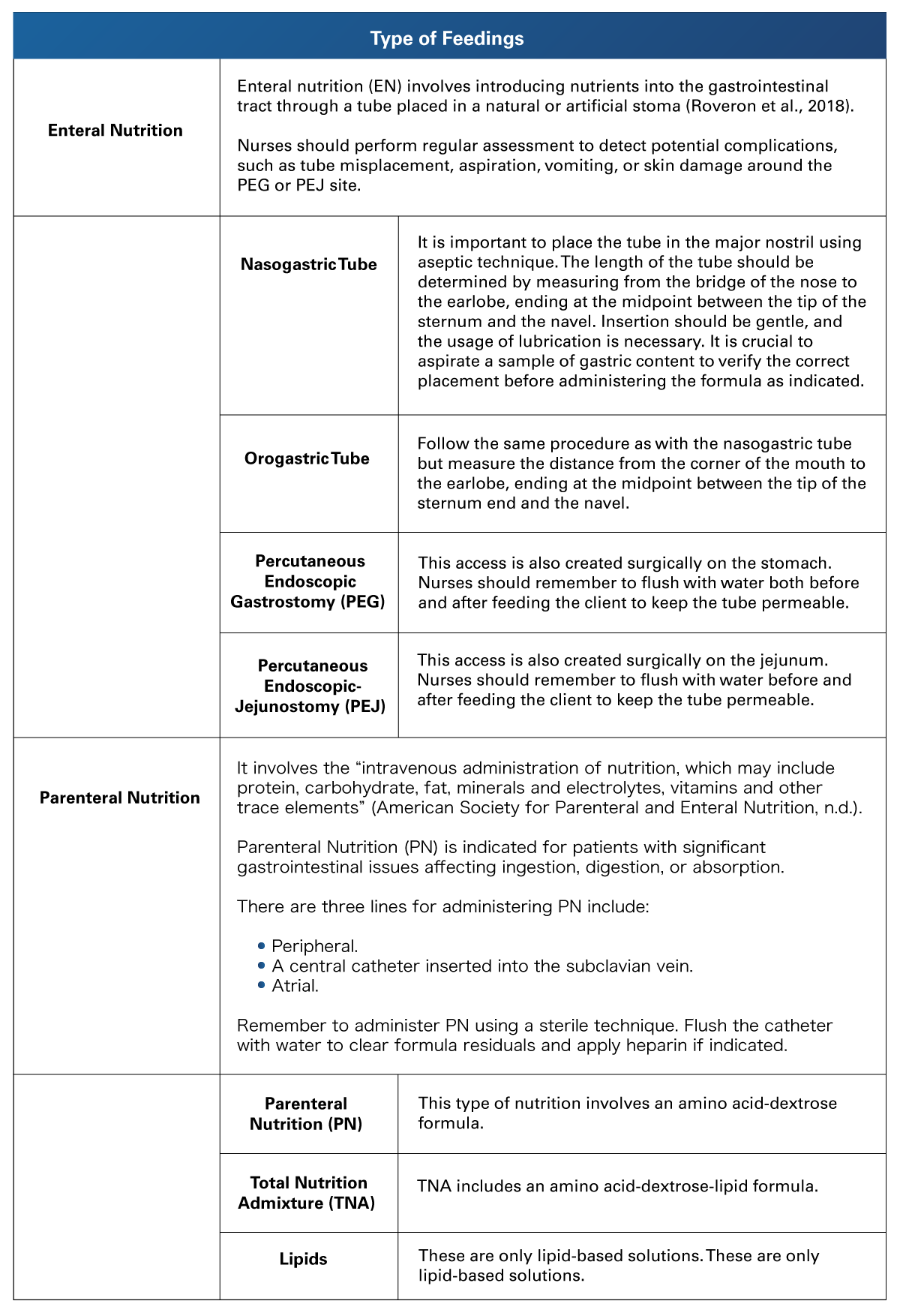 Adapted from American Society for Parental and Enteral Nutrition. (n.d.). What Is Parenteral Nutrition. https://www.nutritioncare.org/about_clinical_nutrition/what_is_parenteral_nutrition/
Adapted from American Society for Parental and Enteral Nutrition. (n.d.). What Is Parenteral Nutrition. https://www.nutritioncare.org/about_clinical_nutrition/what_is_parenteral_nutrition/
Hydration
Hydration can be influenced by external factors, such as environmental temperature, sun exposure, and humidity levels. Internal factors that may impact hydration include sex, age, life stage (with older adults and children being more sensitive), weight, body surface area, body temperature, body composition, respiratory rate, dietary and water intake, episodes of diarrhea, burns, cardiac conditions, renal diseases, hormonal disorders, hepatic conditions, or the use of medications like diuretics or corticoids.
The standard daily fluid requirements for adults typically range from 1800 - 2500 ml/day (Kaplan Nursing, 2023). This is because they excrete between 1500 and 2500 ml in a 24-hour period (with a urinary output of 40 – 80 ml/hr), and they experience insensible losses ranging from 500 to 1000 ml over 24 hours.
It is important to bear in mind that every kilogram gained or lost represents one liter of fluid gained (Silvestri & Silvestri, 2022).
Skin turgor assessment is a useful method for evaluating hydration status. Well-hydrated skin should return to its original position within 3 seconds after lifting a skin fold; delayed recoil suggests dehydration. A properly hydrated tongue should be moist and reddish in color; a whitish tongue may indicate dehydration.
Additional symptoms of dehydration include thirst, fatigue, confusion, headache, abdominal pain, vomiting, and fainting. The latter symptoms include low blood pressure, infrequent urination, or complete absence of urination. Clammy skin, tachycardia, arrhythmia, and convulsive crises are warning signs of electrolyte imbalance. Be mindful of conditions such as hyperkalemia and hypokalemia, hypercalcemia and hypocalcemia, hypernatremia and hyponatremia, hypermagnesemia or hypomagnesemia.
On the contrary, edema is characterized by an excess of fluids or an accumulation of excess fluid in extravascular space. Patients with edema may require diuretics to help eliminate this excess fluid. Edema can be evaluated by pressing a finger against the body surface; the skin should return to its normal color and position in no more than three seconds. Any additional time may indicate the presence of edema. Additional signs of hypervolemia include ascites, dyspnea, and lung crackles.
Pitting edema is defined as “swelling due to excessive accumulation of fluid under the skin, characterized by a persistent indentation when pressure is applied to the swollen area” according to the National Library of Medicine (n.d.). The following formula can help you to identify the grade of edema.
Pitting edema is evaluated and classified as follows:
Table 2
Pitting Edema Classification
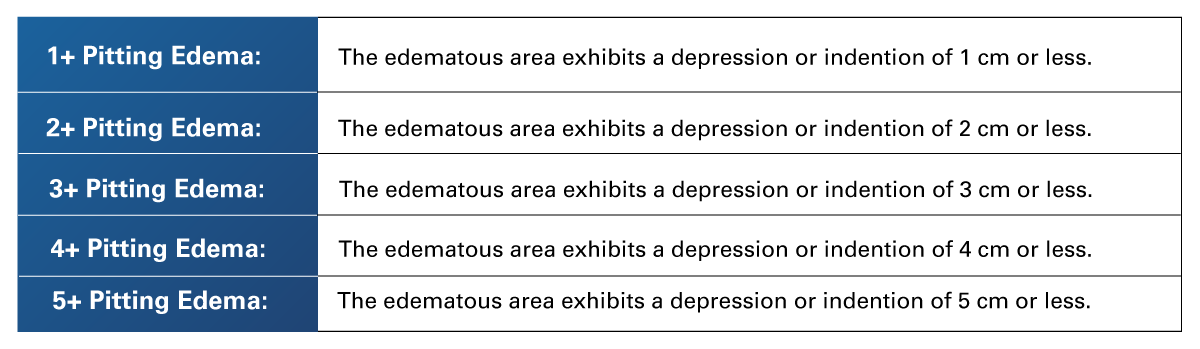 Retrieved from Registered Nursing.org. (2023). Personal Hygiene: NCLEX-RN. https://www.registerednursing.org/nclex/personal-hygiene/
Retrieved from Registered Nursing.org. (2023). Personal Hygiene: NCLEX-RN. https://www.registerednursing.org/nclex/personal-hygiene/
If the client has dehydration, nurses should slowly provide fluids with electrolytes and assess the need for intravenous (IV) fluids administration. In the case of hyperhydration, control fluid intake as necessary (Ernstmeyer & Christman, 2020).
1.3 Rest and Sleep
 Rest and sleep are two crucial components of both mental health and physical health. These periods allow the body to regenerate mental and brain processes, in the case of children and adolescents, sleep helps in growth.
Rest and sleep are two crucial components of both mental health and physical health. These periods allow the body to regenerate mental and brain processes, in the case of children and adolescents, sleep helps in growth.
Sleep is primarily regulated by two principal mechanisms:
- The circadian rhythm: A photosensitive process in which daylight guides the brain to remain awake while darkness signals sleep. It also determines the timing of sleep.
- Sleep-wake homeostasis: It identifies an individual’s need for sleep. This need increases as hours of wakefulness accumulate and results in longer sleep durations following periods of sleep deprivation.
Biological factors that impact sleep factors include age, sex, pregnancy, stress, anxiety, depression, feelings of insecurity, disease, pain, and the effects of medications. Personal factors also play a role, such as inconsistent bedtime schedules, late-night eating, screen time with TV or smart devices before bed, environment noise or light, and discomfort.
Sleep Phases and Stages
Sleep consists of two phases: Rapid Eye Movement (REM) and non-REM sleep. On average, the phases are completed in 80 to 100 minutes, with approximately six cycles occurring per night (Ernstmeyer & Christman, 2020). During the REM stage, sleep occurs with rapid eye movement. Non-REM sleep is further divided into three stages. The first stage follows waking, the second marks the onset of sleep, and the third is characterized by deep sleep.
Nurses should assess sleep pattern disturbances by asking about difficulties falling asleep, restlessness, sleep duration, sleep schedule, and habits. In cases of sleep problems, it is necessary to inquire about symptoms like headaches, irritability, concentration problems, and episodes of microsleep during essential activities like driving, working, cooking, or studying. It is essential to direct questions to identify the potential causes or factors affecting sleep.
Nursing interventions involve guiding clients to adopt healthy sleep habits, including having an early dinner, adhering to a consistent bedtime, creating a relaxing environment to sleep, avoiding exposure to blue light devices like smartphones or TVs before sleep, and addressing risks of injury due to microsleep episodes.
1.4 Nursing Procedures and Psychomotor Skills: Techniques of Physical Assessment (Vital Signs and Head-to-Toe Assessment)
 Assessment is an organized and systematic process for gathering data on the patient's health status from both primary and secondary sources. When conducting an interview, the nurse should introduce themselves to the patient and aim to instill confidence. Providing a private and confidential environment can help the patient feel at ease and cooperate with the assessment.
Assessment is an organized and systematic process for gathering data on the patient's health status from both primary and secondary sources. When conducting an interview, the nurse should introduce themselves to the patient and aim to instill confidence. Providing a private and confidential environment can help the patient feel at ease and cooperate with the assessment.
Physical assessment comprises two phases: data collection (the specific information obtained from the patient) and documentation (recording the data in the patient's record). Registered nurses perform the initial assessment, while advanced practice nurses, such as nurse practitioners and doctors, document all the patient information. Licensed practical nurses then review these details and verify the data with the patient. The collected data includes subjective, objective, historical, and current information. The methods employed for data collection encompass interviews, observations, physical examinations, and medical history.
1. Interview
a) Allows the nurse to obtain specific information necessary for diagnosis and planning.
b) Enhances the nurse-patient relationship and creates an opportunity for dialogue.
c) Empowers the patient to receive information, identify problems, and establish goals.
d) Assists the nurse in identifying areas for further investigation. Anamnesis includes all the patient recalls from their past life regarding their health issues including the reason for the consultation, patient profile, family history, as well as pathological and non-pathological personal history.
2. Physical examination
This is the most crucial method in data collection because the nursing examination focuses on further defining the human response, especially those responses that can be treated with nursing actions. It also establishes a database for comparison when evaluating the effectiveness of nursing interventions and validates the subjective data obtained during the interview. The exploration techniques include inspection, palpation, percussion, and auscultation. The most common exploration method is conducted from head to toe including the following procedures:
- Inspection: This procedure involves visual examination of the client from head to toe, performed in a cephalocaudal manner.
- Palpation: This procedure involves a tactile examination using a sense of touch to assess the client.
- Percussion: This procedure involves tapping the client’s body with the fingers to assess the consistency and size of the tissues and to detect the presence of air or fluid.
- Auscultation: This procedure involves using medical devices and the sense of hearing to listen to sounds, such as those produced by the heart, intestines, and lungs.
According to Ford (2019) the following two mnemonics are useful for assessing symptoms like pain:
- OPQRST stands for Onset, Provokes, Quality, Radiates, Severity, and Time.
- SOCRATES stands for Site, Onset, Character, Radiates, Associations, Timing, Exacerbating factors, and Severity.
3. Vital signs
Vital signs are objective data collected directly from the patient, providing information related to the patient´s level of health. They include Blood Pressure (BP), Heart Rate (HR), Respiratory Rate (RR), and Temperature (T). Vital signs can be influenced by:
- External factors, such as environmental temperature, atmospheric pressure, and the carbon dioxide content in the air.
- Personal factors, including emotions like excitement, anger, sadness, depression, stress, and smoking.
- Biological factors, such as age, sex, exercise, weight, fiber intake, infection, anemia, pain, dehydration, hyperkalemia, hypokalemia, hyperglycemia, hypoglycemia, hormones, narcotics, beta-blockers, calcium channel blockers, and other drugs.
Average values on adults are as follows:
Table 3
Vital Signs
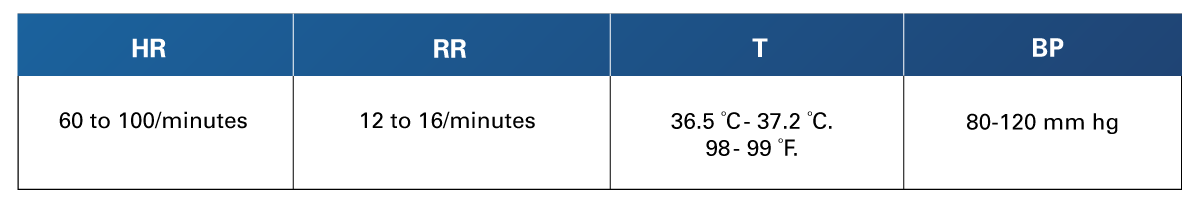 Adapted from Johns Hopkins Medicine. (n.d.). Vital Signs (Body Temperature, Pulse Rate, Respiration Rate, Blood Pressure). https://www.hopkinsmedicine.org/health/conditions-and-diseases/vital-signs-body-temperature-pulse-rate-respiration-rate-blood-pressure
Adapted from Johns Hopkins Medicine. (n.d.). Vital Signs (Body Temperature, Pulse Rate, Respiration Rate, Blood Pressure). https://www.hopkinsmedicine.org/health/conditions-and-diseases/vital-signs-body-temperature-pulse-rate-respiration-rate-blood-pressure
Nurses must use the appropriate technique and medical devices suitable for the patient’s characteristics to obtain reliable data. Specific recommendations are provided as follows:
HR. Detect the pulse in correct places (radial, carotid, femoral, brachial, temporal, apical, popliteal, tibial) for one minute to assess strength, uniformity, pattern changes, and rate.
RR. Count ventilations for one minute and document frequency, depth, pace, and effort.
T. Place the thermometer following the manufacturer's instructions and according to the patient's characteristics.
BP. Use the appropriate sphygmomanometer and stethoscope for each patient. Remember to place the stethoscope over the artery so you can document the first and last pulse sounds. Avoid placing the cuff on or near injuries, surgeries, intra-arterial lines, or dialysis shunts.
 In conclusion, it is essential to remember that the activities of daily living form the foundation of an individual’s development. Losing the ability to perform basic tasks such as eating, drinking, resting and sleeping can have a significant impact on a person's life if they are not adequately assisted or supported. Employ techniques and methods to assess client needs and health conditions, keeping in mind that the client is a biological, psychosocial, and spiritual person.
In conclusion, it is essential to remember that the activities of daily living form the foundation of an individual’s development. Losing the ability to perform basic tasks such as eating, drinking, resting and sleeping can have a significant impact on a person's life if they are not adequately assisted or supported. Employ techniques and methods to assess client needs and health conditions, keeping in mind that the client is a biological, psychosocial, and spiritual person.
Providing the necessary assistance not only addresses immediate needs but also helps prevent complications that may arise from the disability and contributes to the client's overall state of well-being and health.
- American Society for Parenteral and Enteral Nutrition. (n.d.). What Is Parenteral Nutrition. https://www.nutritioncare.org/about_clinical_nutrition/what_is_parenteral_nutrition/
- Ernstmeyer, K., & Christman, E. (2020). Nursing Fundamentals. Chippewa Valley Technical College. https://www.ncbi.nlm.nih.gov/books/NBK591820/
- Ford, C. (2019). Adult Pain Assessment and Management. British Journal of Nursing, 28(7), 421-423. https://www.britishjournalofnursing.com/content/clinical/adult-pain-assessment-and-management/
- Johns Hopkins Medicine. (n.d.). Vital Signs (Body Temperature, Pulse Rate, Respiration Rate, Blood Pressure). https://www.hopkinsmedicine.org/health/conditions-and-diseases/vital-signs-body-temperature-pulse-rate-respiration-rate-blood-pressure
- Kaplan Nursing. (2023). NCLEX-RN Content review Guide (9th ed.). Kaplan Test Prep.
- Nasiri, M., Jafari, Z., Rakhshan, M., Yarahmadi, F., Zonoori, S., Akbari, F., Sadeghi Moghimi, E., Amirmohseni, L., Abbasi, M., Keyvanloo Sharstanaki, S., & Rezaei, M. (2022). Application of Orem's Theory-based Caring Programs Among Chronically Ill Adults: A Systematic Review and Dose-response Meta-analysis. International Nursing Review, 70(1), 59–77. https://doi.org/10.1111/inr.12808
- National Library of Medicine. (n.d.). Pitting edema. https://www.ncbi.nlm.nih.gov/medgen/137681
- Registered Nursing.org. (2023, September 23). Personal Hygiene: NCLEX-RN. https://www.registerednursing.org/nclex/personal-hygiene/
- Roveron, G., Antonini, M., Barbierato, M., Calandrino, V., Canese, G., Chiurazzi, L. F., Coniglio, G., Gentini, G., Marchetti, M., Minucci, A., Nembrini, L., Neri, V., Trovato, P., & Ferrara, F. (2018). Clinical Practice Guidelines for the Nursing Management of Percutaneous Endoscopic Gastrostomy and Jejunostomy (PEG/PEJ) in Adult Patients: An Executive Summary. Journal of Wound, Ostomy, and Continence Nursing, 45(4), 326–334. https://doi.org/10.1097/WON.0000000000000442
- Silvestri, L. A., & Silvestri, A. E. (2022). Saunders Comprehensive Review for the NCLEX-PN Examination (9th ed.). Elsevier.
- Tanaka, M. (2022). Orem's Nursing Self-care Deficit Theory: A Theoretical Analysis Focusing on its Philosophical & Sociological Foundation. Nursing Forum, 57(3), 480–485. https://doi.org/10.1111/nuf.12696
- University of Nebraska Medical Center. (n.d.). Interventions to Reduce Risk for Patients with Toileting Needs. https://www.unmc.edu/patient-safety/capturefalls/roadmap/interventions/toileting/index.html
The following links do not belong to Tecmilenio University, when accessing to them, you must accept their terms and conditions.
Readings
- Ford, C. (2019). Adult Pain Assessment and Management. British Journal of Nursing, 28(7), 421-423. https://www.britishjournalofnursing.com/content/clinical/adult-pain-assessment-and-management/
- USDA. (n.d.). Dietary Guidelines for Americans 2020-2025. Executive summary. https://www.dietaryguidelines.gov/sites/default/files/2021-03/DGA_2020-2025_ExecutiveSummary_English.pdf
Videos
- DrBruce Forciea. (2017, April 21). Fluids and electrolytes: Water [Video]. YouTube. https://youtu.be/VMxmDeduKR0?si=Eo97SmY9ufJtcSmb
- Provincial Health Services Authority (PHSA). (2018, December 12). Hooking up to Parenteral Nutrition [Video]. YouTube. https://www.youtube.com/watch?v=iVruV_9M-Ns
- NCLEX Practice Questions by NURSIGNCOM. (2016, July 11). NCLEX Practice Questions: Calorie Counting for Weight Loss (GI/GU/Basic Care and Comfort) [Video]. YouTube. https://www.youtube.com/watch?v=UDyc-oWhO_4
La obra presentada es propiedad de ENSEÑANZA E INVESTIGACIÓN SUPERIOR A.C. (UNIVERSIDAD TECMILENIO), protegida por la Ley Federal de Derecho de Autor; la alteración o deformación de una obra, así como su reproducción, exhibición o ejecución pública sin el consentimiento de su autor y titular de los derechos correspondientes es constitutivo de un delito tipificado en la Ley Federal de Derechos de Autor, así como en las Leyes Internacionales de Derecho de Autor.
El uso de imágenes, fragmentos de videos, fragmentos de eventos culturales, programas y demás material que sea objeto de protección de los derechos de autor, es exclusivamente para fines educativos e informativos, y cualquier uso distinto como el lucro, reproducción, edición o modificación, será perseguido y sancionado por UNIVERSIDAD TECMILENIO.
Queda prohibido copiar, reproducir, distribuir, publicar, transmitir, difundir, o en cualquier modo explotar cualquier parte de esta obra sin la autorización previa por escrito de UNIVERSIDAD TECMILENIO. Sin embargo, usted podrá bajar material a su computadora personal para uso exclusivamente personal o educacional y no comercial limitado a una copia por página. No se podrá remover o alterar de la copia ninguna leyenda de Derechos de Autor o la que manifieste la autoría del material.