Basic Care and Comfort / 03
Make sure to:
- Retain the necessary knowledge for assessing the needs related to mobility or immobility in patients/clients.
- Identify the appropriate techniques and methods for evaluating mobility or immobility needs.
- Implement evidence-based nursing interventions to manage mobility or immobility issues.
 Picture the following example: a patient has undergone shoulder surgery and is now home on their first day after being discharged. They want to go back to their normal life, but they find that even the simpler tasks are now hard to do. They experience complicated feelings because they now need to wait for others to help them out or face the embarrassment of others witnessing their struggle to do things themselves. They wonder if they will be able to move like they used to and are worried about how long that might take.
Picture the following example: a patient has undergone shoulder surgery and is now home on their first day after being discharged. They want to go back to their normal life, but they find that even the simpler tasks are now hard to do. They experience complicated feelings because they now need to wait for others to help them out or face the embarrassment of others witnessing their struggle to do things themselves. They wonder if they will be able to move like they used to and are worried about how long that might take.
Mobility is vital for an individual's well-being and quality of life, allowing them to perform daily activities such as going to work, attending school, participating in leisure activities, and engaging in physical exercise. The total or partial loss of mobility significantly impacts an individual’s development, leading to dependence on medical devices or assistance from others. Nurses must be able to identify alterations in mobility and investigate the underlying causes in order to aid in their recovery, maintenance, rehabilitation, or adaptation to these changes.
External factors affecting movement include aspects such as environmental temperature, patient height, and weight. For instance, the skin is influenced by external factors like temperature, light, humidity, and environmental pollution. Internal factors that can affect either movement or skin condition encompass the patient's age, sex, hereditary traits, overall health, nutritional status, existing pathologies, accidental injuries, and medication usage.
2.1 Assessment of Mobility and Skin

Movement Assessment
 Movement assessment involves observing the range of motion in the joints, as well as evaluating the patients'/clients' strength, skill, and cardiovascular endurance.
Movement assessment involves observing the range of motion in the joints, as well as evaluating the patients'/clients' strength, skill, and cardiovascular endurance.
- Motion. Strength, speed, flexibility, endurance, and range of motion observed in daily activities or specific exercises, in addition to walking.
- Body Control Ability. Organization, coordination, balance, flexibility, and agility.
- Cardiovascular resistance. Adaptations related to respiratory and cardiac function, as well as integumentary coloration.
There are different moments when the nurse can evaluate the patient’s/client’s movement. Some examples would be:
- During tasks explicitly assigned for evaluation.
- While the patient/client is engaged in activities of daily living such as walking, eating, bathing, or dressing.
- When the patient/client is sitting.
- When the patient/client is lying down.
When describing movement, it is important to provide the context of the patient’s/client’s position while carrying it out. The most common natural body postures are:
- Supine position. Lying on the back.
- Prone position. Lying on the abdomen.
- Lateral decubitus. Lying on the right or left side.
- Standing. Upright on the feet.
- Sitting. Upright in a chair.
Skin Assessment
 Skin assessment involves observing appearance, color, turgor, edema, wounds or ulcers, and infections.
Skin assessment involves observing appearance, color, turgor, edema, wounds or ulcers, and infections.
- Color. For light-skinned patients, the physiological skin color varies in shades of pink. Pale skin can signify anemia or low blood pressure, while blue might indicate an oxygen deficiency. Red may point to high blood concentration or inflammation, and black signifies dead tissue. To assess capillary refill, press two fingers against the client's nail until it turns pale; the color should return in less than three seconds under normal conditions.
- Turgor. The skin should be firm and elastic, allowing it to return to its original position when moved or pulled. Loss of turgor may result from advanced age, dehydration, or edema. To assess, pinch the skin; it should revert to its original position in less than three seconds. If it takes longer, this could indicate dehydration.
- Edema. This condition is characterized by fluid accumulation in the extracellular space. To assess edema, press the tip of the index finger against the tissue and observe whether the indentation remains.
Wounds
While assessing the skin, another aspect that the nurse should be able to properly describe are the noticeable wounds that the patient/client could present.
Wounds are considered as any damage to the tissues, and can be classified as follows:
- Closed wounds. These wounds do not result in a loss of skin continuity but involve damage to the underlying tissues.
- Open wounds. In these wounds, the skin is open, allowing communication between the underlying tissues and the outside.
- Linear wounds. These open wounds can quickly have their skin edges aligned.
- Irregular wounds. These are open wounds with non-coinciding skin edges due to irregular or jagged borders.
- Abrasive wounds. These wounds are caused by friction.
- Avulsion wounds. These wounds involve partial tissue amputation.
- Total amputation. This type of wound results in the loss of a limb.
- Wounds from a sharp weapon. In these wounds, a sharp object breaks the skin, and the object may be either inside or outside the wound.
- Wounds by a firearm. These wounds exhibit an entrance hole with inverted and irregular edges. If the shot is fired from close range, the wound may have a peripheral ring of gunpowder burn. The exit orifice features irregular externalized edges, usually more prominent than the entry orifice.
- First-degree burn wounds. These wounds affect the dermis, causing the skin to become red.
- Second-degree burn wounds. These wounds affect both the dermis and epidermis. The skin becomes red, and blisters are present.
- Third-degree burn wounds. These wounds affect the dermis, epidermis, and adjacent cellular tissue, with the possibility of muscle involvement.
- Fourth-degree burn wounds. These wounds affect the dermis, epidermis, adjacent cellular tissue, muscle, and bone.
- Infected wounds. These wounds present signs such as redness, pain, heat, inflammation, and collection of whitish secretions due to the presence of white blood cells.
While attending to patients or clients with wounds, understanding the different types of wound healing provides nurses with a framework for knowing how care should be administered. The types of wound healing are as follows:
- Primary Intention Healing. In this type, the wound closes on its own after the injury has occurred.
- Secondary Intention Healing. In this case, the wound must be opened again due to the presence of an infection. After controlling the infection, it is closed back.
- Tertiary Intention Healing. This occurs when the wound must be reopened multiple times to manage the infection.
A particular type of skin wound prevalent among patients with mobility challenges is the pressure ulcer. Due to immobility and continuous friction in their resting postures, there is diminished blood circulation, leading to tissue detachment. This leads to breaks in the skin layers and the risk of infections is increased.
To assess the risk of developing ulcers, clinicians commonly utilize the Braden Scale. In this scale, each item is scored from 1 to 4, as shown in the table that follows.
Table 1
Braden Scale for Predicting Pressure Sore Risk
 Retrieved from Kennerly et al. (2022). Nursing Assessment of Pressure Injury Risk with the Braden Scale Validated against Sensor-Based Measurement of Movement. Healthcare, 10(11). https://doi.org/10.3390/healthcare10112330
Retrieved from Kennerly et al. (2022). Nursing Assessment of Pressure Injury Risk with the Braden Scale Validated against Sensor-Based Measurement of Movement. Healthcare, 10(11). https://doi.org/10.3390/healthcare10112330
Based on their appearance and extent, pressure ulcers can be categorized into various stages, as shown in the table below:
Table 2
Ulcer Classification
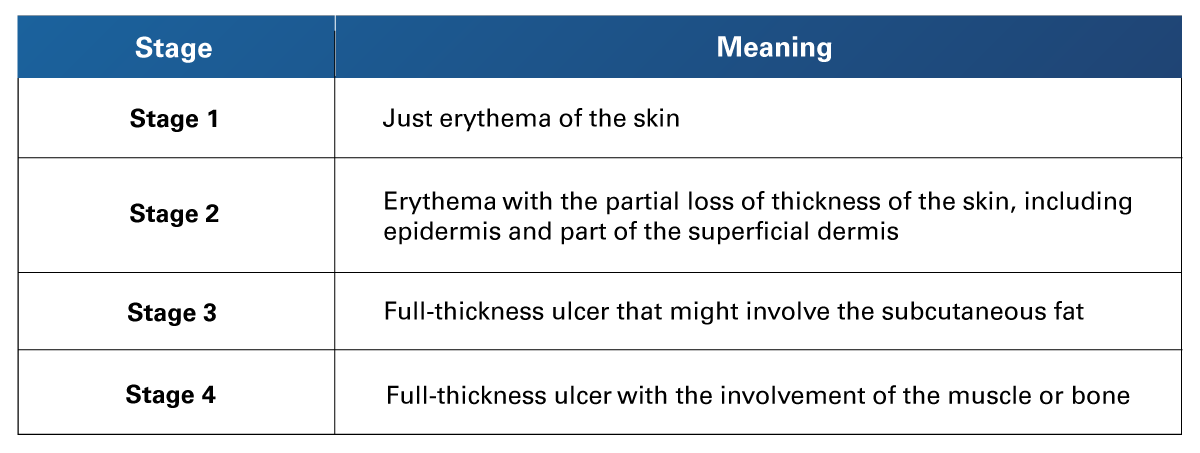 Retrieved from Aboud, A., & Manna, B. (2023). Wound Pressure Injury Management. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532897/
Retrieved from Aboud, A., & Manna, B. (2023). Wound Pressure Injury Management. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532897/
2.2 Identification of immobility complications
 Immobility has a significant impact on various body systems. Understanding the unique characteristics of these systems and how their alterations are interconnected provides nurses with the knowledge required to deliver specific care to their patient/client.
Immobility has a significant impact on various body systems. Understanding the unique characteristics of these systems and how their alterations are interconnected provides nurses with the knowledge required to deliver specific care to their patient/client.
Musculoskeletal System
Due to a lack of movement, bones experience calcium loss, increasing the risk of fractures and subsequent falls. Joints become stiff, resulting in a reduced range of motion, and may also show signs of inflammation. Muscles weaken and are prone to atrophy.
Integumentary System
Pressure on weight-bearing areas of the body —such as the scapulae, sacrum, ischium, and heels— interrupts blood flow. This leads to symptoms like redness, irritation, poor skin turgor, edema, and pain, along with a loss of skin integrity. These conditions can evolve into more severe complications like ulcers, osteomyelitis, necrotizing fasciitis, gas gangrene, or septicemia.
Circulatory System
Prolonged immobility leads to a loss of muscle tone, which in turn affects the tone of blood vessels. This can result in dilated vessels, causing both resting hypotension and orthostatic hypotension, thereby increasing the patient's/client’s risk of falls. Slow blood flow heightens the risk for varicose veins, thrombophlebitis, and emboli. Moreover, the leakage of intravascular fluid into the extravascular space can cause edema, potentially progressing to cellulitis, ulcers, and necrosis. To compensate for stasis, the heart works harder, often leading to late-stage ventricular hypertrophy and other complications related to preload and afterload imbalances.
Respiratory System
Fluid leakage from the intravascular space into the lung's interstitial space can result in respiratory distress, coughing, increased secretions, and heightened risk of infection, including conditions like atelectasis and pneumonia.
Gastrointestinal System
Gastrointestinal movements decrease in force and frequency, so constipation and compaction may appear.
Urinary System
Urine stagnation promotes the formation of stones as solutes settle. This static condition also fosters bacterial and viral replication, increasing the likelihood of infection. Delayed bladder emptying can further contribute to urinary incontinence.
Metabolic System
The metabolic rate diminishes, potentially leading to weight gain. Furthermore, constipation may contribute to anorexia and inadequate nutrient intake.
Psychological Alterations
Emotional well-being significantly influences an individual's quality of life. Long-term or even permanent loss of mobility could engender depression. The feelings of dependency, coupled with the absence of a robust support network, could exacerbate this condition.
2.3 Care Interventions to Promote and Assist Patient/Client Safety, Mobility, Circulation, and Skin Integrity
 As part of the comprehensive care provided by nurses, there exists a suite of interventions designed to identify, manage, and mitigate the afflictions discussed, along with their potential complications.
As part of the comprehensive care provided by nurses, there exists a suite of interventions designed to identify, manage, and mitigate the afflictions discussed, along with their potential complications.
General Nursing Interventions that should be routinely applied include:
- Assessing and treating pain.
- Evaluating mental state and, if necessary, referring the patient/client to psychological services.
- Evaluating and engaging the patient's/client's social support network.
- Assessing housing resources and recommending necessary adaptations.
- Promoting or assisting in proper nutrition and hydration.
- Maintaining or encouraging a healthy weight.
Interventions to Promote Mobility include:
- Promoting or assisting in joint movement exercises for maximum range of motion (ROM).
- Promoting or assisting in fine motor exercises.
- Promoting or assisting in muscular resistance exercises.
- Encouraging or simulating walking, depending on the patient's ability.
- Providing percussive therapy to the patient.
Some Interventions to Promote Circulation are:
- Limiting prolonged periods of sitting or standing.
- Elevating legs to approximately 30 degrees following extended periods of inactivity.
- Administering massages with centripetal movements.
- Adapting compression stockings progressively to the patient.
- Utilizing the Trendelenburg position for hypotensive episodes.
- Promoting or assisting in a variety of exercises, including aerobic, symmetrical, resistance, and compression.
- Advising cessation of smoking.
- Encouraging early mobility post-surgery to mitigate thrombosis risk.
The Interventions to Promote Skin Integrity include:
- Ensuring or assisting in wrinkle-free bed-making.
- Promoting or assisting in daily hygiene practices.
- Avoiding irritants like harsh soaps, scrubs, and alcohol-based lotions.
- Preventing high-humidity conditions, particularly in skin and genital folds.
- Applying moisturizing creams.
- Promoting or assisting in frequent postural changes.
- Utilizing supportive cushions to distribute body weight and maintain alignment.
- Implementing alternating pressure mattresses for even weight distribution.
- Promoting or assisting in body massages.
- Conducting daily assessments for ulcer risk.
- Adapting therapeutic positioning to align with the treatment plan.
Some therapeutic positions are:
- Fowler's Position: The patient/client is seated, with the bed angle set between 45 and 60 degrees. The legs may be either straight or slightly bent.
- Semi-Fowler Position: The patient/client lies on their back, with the head of the bed elevated to an angle of 30 to 45 degrees.
- Trendelenburg Position: The patient/client lies in a supine position, with the upper limbs elevated at 45 degrees.
- Inverted Trendelenburg: The patient/client assumes a supine position, with their head elevated at 45 degrees.
- Spinal or Lumbar Position: The patient/client adopts a fetal position while in lateral decubitus, either on the right or left side.
When pressure ulcers have been developed, the need for debridement might arise. Various types of debridement exist, each with its own specific technique tailored to the nature of the wound. These types include:
- Mechanical Debridement: This technique involves the removal of dead cells and purulent secretions through friction. Materials such as hydrogels, hydrocolloids, or saline-moistened gauze are commonly used.
- Negative-Pressure Wound Therapy: This therapy inhibits the passage of oxygen to the ulcer by covering it with a specialized bandage.
- Autolytic Debridement: A transparent film is applied to maintain a moisture-rich environment, allowing the body's natural enzymes to conduct the debridement.
- Enzymatic Chemical Debridement: Exogenous enzymes are applied to the eschar, initiating the breakdown process.
- Recombinant Platelet-Derived Growth Factors: This method stimulates the growth of new tissue.
- Sharp Instrument Debridement: Dead cells are excised using sharp instruments in this technique.
- Surgical Debridement: A laser is employed to remove necrotic tissue.
- Ultrasound Debridement: Soft waves penetrate tissues to stimulate blood flow.
- Hyperbaric Oxygen Therapy: This technique requires a special chamber where 100% oxygen is supplied.
2.4 Management of Assistive Devices for Mobility and Immobility
Medical Devices to Manage Mobility and Immobility Issues
 Due to immobility, patients/clients may require specialized medical devices to facilitate their daily activities. Below are the most frequently employed:
Due to immobility, patients/clients may require specialized medical devices to facilitate their daily activities. Below are the most frequently employed:
Walking Stick. The cane should be used on the affected side, keeping the elbow at an angle between 25 to 30 degrees. The cane should be positioned 15 cm from the side of the foot. When advancing, extend the cane 30 cm forward and then step.
Walker. Position the walker comfortably in front of the patient. Instruct the patient/client to advance the walker approximately 15 cm with each step.
Crutches. Place the crutches 15 cm beside and ahead of the foot. When stepping, the crutch on the affected side should lead. The hands should bear the body weight via the crutch handles, with the elbow angled at 25 to 30 degrees.
Gait Belt. This belt serves as a handle, easing the process of moving the patient.
Slider Boards. Utilized to slide patients from one position to another, these boards reduce surface friction.
Sit-to-Stand Lifts. These facilitate the patient's transition from sitting to standing positions.
Mechanical Lift. Particularly useful for patients who are either fully immobile or overweight, this device helps in relocating them.
Splints. Employed to immobilize limbs in cases of fractures or sprains. Ensure there is finger-width space between the splint and the skin and monitor blood circulation in the nail bed as previously described. For arm splints, elevation can minimize swelling.
Medical Traction Equipment. A system of weights and pulleys designed to provide spacing or alignment for bones or joints.
Braces. Used to provide support and alignment for various body parts, common types include neck, back, and elbow braces.
Medical Devices to Promote Circulation

Compression Socks. These firm, reinforced socks are designed to prevent blood stagnation and edema. The degree of compression should be gradually adjusted to assess patient/client tolerance.
Intermittent Pneumatic Compression (IPC). This system consists of air cuffs wrapped around the legs to apply pressure, thereby preventing edema and stimulating circulation.
Blood Circulation Machine for Arms or Legs. These devices employ repetitive movements to stimulate blood circulation in the extremities.
Medical Devices to Manage Skin Integrity

Pillows and Wedges. Utilized for body alignment and pressure distribution, these aids help vary body positions to disperse weight at different pressure points.
Chair Cushions. Especially useful for wheelchair users who are prone to bedsores, these cushions alleviate body weight pressure on the ischium and mitigate the risk of ulcers.
Mattresses Toppers. Also known as bed covers or Egg Crate covers, these provide an extra layer for skin care (Mansouri, 2023).
Soft Mattresses. Recommended for minimizing skin pressure, these mattresses are more effective than their orthopedic counterparts for this purpose.
Air Mattress. Serving as a pressure-relief mechanism, these mattresses are designed to reduce the body weight's impact on pressure points.
Alternating Pressure Mattresses. These advanced mattresses are engineered to periodically shift the distribution of body weight, offering an additional level of pressure relief.
 Recalling the initial example of the patient who underwent shoulder surgery, it is now evident that his temporary state of immobility can induce emotional distress and impact both his quality of life and overall health. At the same time, learners should understand that this condition can be holistically managed. It can be evaluated, monitored, and most importantly, mitigated through proper intervention. A skilled nurse can implement any of the interventions discussed in this unit to provide the necessary comfort and expedite the healing process for underlying conditions. Meticulous attention to detail in detecting and treating any skin lesions is also a vital component of exceptional nursing care, one that facilitates quicker recovery, rehabilitation, and functional maintenance. Involving the family to establish a robust support network will undoubtedly yield significant benefits in patient care.
Recalling the initial example of the patient who underwent shoulder surgery, it is now evident that his temporary state of immobility can induce emotional distress and impact both his quality of life and overall health. At the same time, learners should understand that this condition can be holistically managed. It can be evaluated, monitored, and most importantly, mitigated through proper intervention. A skilled nurse can implement any of the interventions discussed in this unit to provide the necessary comfort and expedite the healing process for underlying conditions. Meticulous attention to detail in detecting and treating any skin lesions is also a vital component of exceptional nursing care, one that facilitates quicker recovery, rehabilitation, and functional maintenance. Involving the family to establish a robust support network will undoubtedly yield significant benefits in patient care.
- Aboud, A., & Manna, B. (2023). Wound Pressure Injury Management. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532897/
- Kennerly, S. M., Sharkey, P. D., Horn, S. D., Alderden, J., & Yap, T. L. (2022). Nursing Assessment of Pressure Injury Risk with the Braden Scale Validated Against Sensor-based Measurement of Movement. Healthcare, 10(11). https://doi.org/10.3390/healthcare10112330
- Mansouri, M., Krishnan, G., McDonagh, D., Zallek, C., & Hsiao-Wecksler, E. (2023). Review of Assistive Devices for the Prevention of Pressure Ulcers: An Engineering Perspective. Disability and Rehabilitation: Assistive Technology. https://doi.org/10.1080/17483107.2023.2204127
The following links do not belong to Tecmilenio University, when accessing to them, you must accept their terms and conditions.
Readings
- Cleveland Clinic. (2023). Bedsores (Pressure Injuries). https://my.clevelandclinic.org/health/diseases/17823-bedsores-pressure-injuries
Videos
- Cleveland Clinic. (n.d.). At Home Care for Your Pressure Injuries [Video]. https://cdnapisec.kaltura.com/index.php/extwidget/preview/partner_id/2207941/uiconf_id/37292221/entry_id/0_6233ayzg/embed/dynamic
- Mayo Clinic. (2020, March 30). Passive Motion Exercises [Video]. YouTube. https://www.youtube.com/watch?v=EjJ5nX_jM-w
La obra presentada es propiedad de ENSEÑANZA E INVESTIGACIÓN SUPERIOR A.C. (UNIVERSIDAD TECMILENIO), protegida por la Ley Federal de Derecho de Autor; la alteración o deformación de una obra, así como su reproducción, exhibición o ejecución pública sin el consentimiento de su autor y titular de los derechos correspondientes es constitutivo de un delito tipificado en la Ley Federal de Derechos de Autor, así como en las Leyes Internacionales de Derecho de Autor.
El uso de imágenes, fragmentos de videos, fragmentos de eventos culturales, programas y demás material que sea objeto de protección de los derechos de autor, es exclusivamente para fines educativos e informativos, y cualquier uso distinto como el lucro, reproducción, edición o modificación, será perseguido y sancionado por UNIVERSIDAD TECMILENIO.
Queda prohibido copiar, reproducir, distribuir, publicar, transmitir, difundir, o en cualquier modo explotar cualquier parte de esta obra sin la autorización previa por escrito de UNIVERSIDAD TECMILENIO. Sin embargo, usted podrá bajar material a su computadora personal para uso exclusivamente personal o educacional y no comercial limitado a una copia por página. No se podrá remover o alterar de la copia ninguna leyenda de Derechos de Autor o la que manifieste la autoría del material.