Pharmacological and Parental Therapies / 04
Make sure to:
- Understand the route of administration for each therapy and familiarize yourself with potential side effects or adverse reactions pertinent to specific patients.
- Identify the key aspects of patient education/information required to support the patient/client in successfully managing their treatment regimen.
- Act as an advocate for the patient, conveying any potential implications of drug therapy to the broader healthcare team in the patient's/client's best interest.
 Imagine a nurse during a busy shift, running from room to room, and in and out of the nurses’ station. While trying to remember the dobutamine order for one of their patients, she overhears a colleague mentioning a recent study about dopamine. Meanwhile, a doctor is speaking loudly on the phone, inquiring about a dose of depo-medrol, and a student asks another if it is related to solu-medrol. There are many drug names that a nurse must know and comprehend to feel secure when treating their patients. Understanding at least which system these drugs pertain to provides a sense of confidence for healthcare professionals.
Imagine a nurse during a busy shift, running from room to room, and in and out of the nurses’ station. While trying to remember the dobutamine order for one of their patients, she overhears a colleague mentioning a recent study about dopamine. Meanwhile, a doctor is speaking loudly on the phone, inquiring about a dose of depo-medrol, and a student asks another if it is related to solu-medrol. There are many drug names that a nurse must know and comprehend to feel secure when treating their patients. Understanding at least which system these drugs pertain to provides a sense of confidence for healthcare professionals.
While the pharmacology of each system can be wide and complex, healthcare professionals should at least be familiar with the most frequently administered medications, as well as their side effects, presentation, and dosing, to promote patient/client compliance and safety with these drugs.
2.1 Cardiovascular and Respiratory System
 There is a variety in the types of medications that can be ordered to control or prevent limiting heart conditions. Two of the most used groups are antihypertensives and antiarrhythmics. Antihypertensives are primarily composed of angiotensin converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), calcium channel blockers and beta blockers. Antiarrhythmics are classified into classes 1 through 4.
There is a variety in the types of medications that can be ordered to control or prevent limiting heart conditions. Two of the most used groups are antihypertensives and antiarrhythmics. Antihypertensives are primarily composed of angiotensin converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), calcium channel blockers and beta blockers. Antiarrhythmics are classified into classes 1 through 4.
Antihypertensives
- ACE Inhibitors: Play a key role in inhibiting the RAAS system (Renin-Angiotensin-Aldosterone System), the system that effectively manages blood pressure when it is low. It operates by inhibiting the body’s production of Angiotensin II which causes vasoconstriction and triggers the release of aldosterone elevating sodium and water into circulation. The result is an increased volume and, consequently, elevated blood pressure; in this case, an ACE inhibitor would cause the opposite effect, which is to lower blood pressure (Liu & Yang, 2019).
- ARBs: Also target the Renin-Angiotensin-Aldosterone system. These medications block vasoconstriction and aldosterone's effects on angiotensin II in numerous sites (vascular smooth muscle and adrenal glands), thereby preventing an elevation in blood pressure (Liu & Yang, 2019).
- Calcium Channel Blockers: Block L-Type calcium channels in the vascular smooth muscle, cardiac myocytes and cardiac nodal tissue. By blocking this channel, they inhibit calcium ion influx during cardiac depolarization. This results in decreased SA/AV node conduction, thereby slowing the heart rate (Liu & Yang, 2019).
- Beta Blockers: Block the beta receptors in the body so that norepinephrine and epinephrine cannot bind with the beta receptors in the body. Catecholamines play a significant role in the sympathetic nervous system. By blocking them, beta blockers slow heart rate, subsequently lowering blood pressure and reducing oxygen consumption during myocardial contractions (Liu & Yang, 2019).
Antiarrhythmics
- Class I: Is divided into Ia, Ib, and Ic. Ia work by causing a moderate degree of blockage of fast sodium channels. They are indicated in premature beats, atrial flutter or atrial fibrillation. Ib causes mild degree of blockage of sodium channels, and is recognized for shortening the QTc interval, and is used for Ventricular Arrhythmias only, specifically post-myocardial infarction. Ic results in a pronounced blockage of sodium channels. It is suitable for patients without structural or ischemic heart diseases but with symptomatic supraventricular tachycardia (SVT).
- Class II: Are among the main therapies used in the treatment of heart rate control in patients with paroxysmal, persistent, or permanent atrial fibrillation and atrial flutter (Liu & Yang, 2019).
- Class III Agents: Diminish the exit of potassium from the cell and prolongs the QTc interval. They are indicated in the treatment of ventricular dysrhythmias.
- Class IV Agents: Work by reducing the conduction velocity and slowing the conduction through the AV node. Indicated for supraventricular dysrhythmias (Liu & Yang, 2019).
Table 1
Cardiovascular Medication
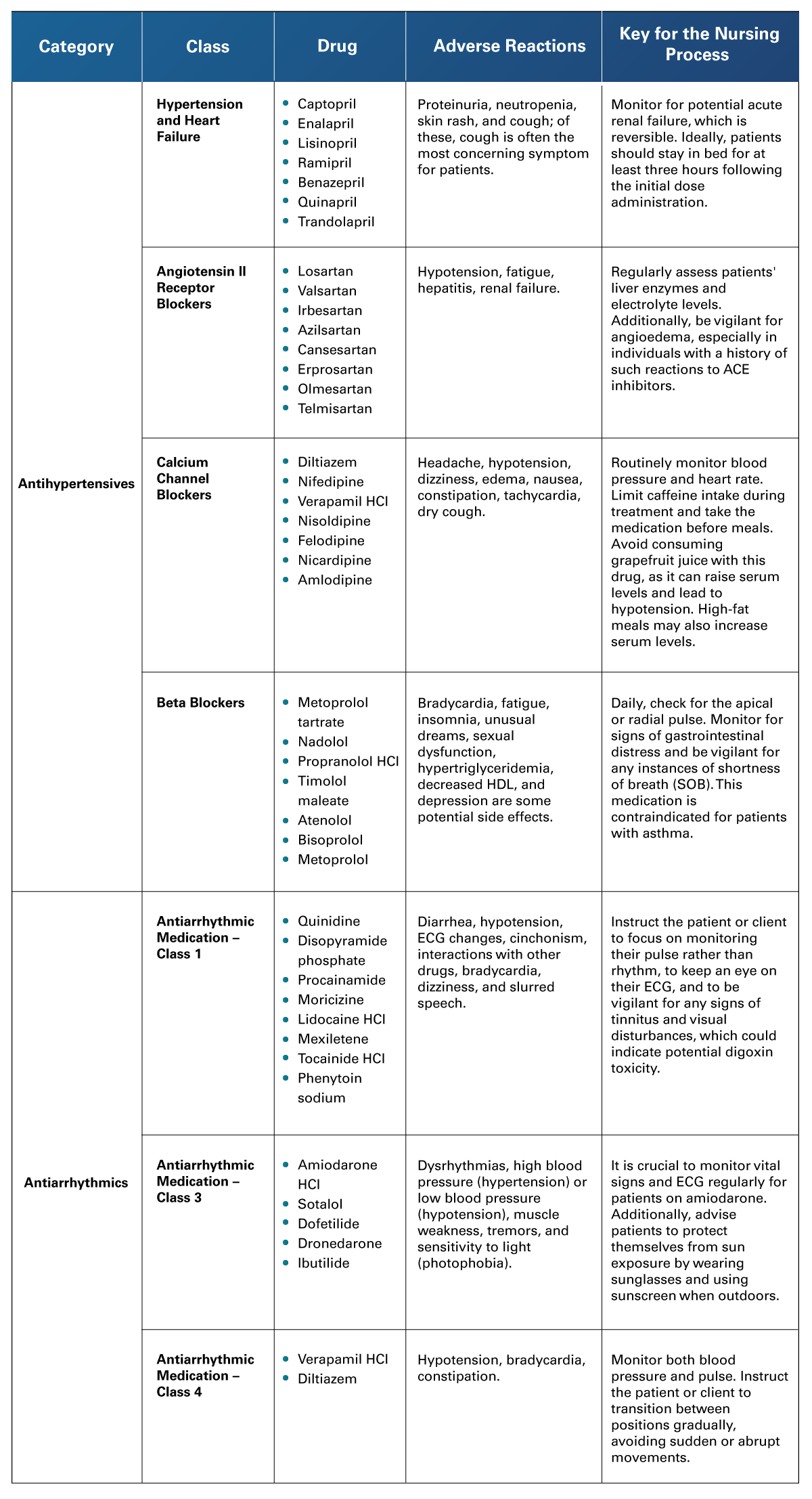 Adapted from Liu, Z., & Yang, B. (2019). Drug Development Strategy for Type 2 Diabetes: Targeting Positive Energy Balances. Curr Drug Targets, 20(8). http://doi.org/10.2174/1389450120666181217111500; Spechler, S.J. (2019). Proton Pump Inhibitors: What the Internist Needs to Know. Med Clin North Am. https://pubmed.ncbi.nlm.nih.gov/30466666/
Adapted from Liu, Z., & Yang, B. (2019). Drug Development Strategy for Type 2 Diabetes: Targeting Positive Energy Balances. Curr Drug Targets, 20(8). http://doi.org/10.2174/1389450120666181217111500; Spechler, S.J. (2019). Proton Pump Inhibitors: What the Internist Needs to Know. Med Clin North Am. https://pubmed.ncbi.nlm.nih.gov/30466666/
Regarding medication for the respiratory system, bronchodilators are a significant part of the market. They are prescribed for patients/clients who have suboptimal airflow through the lungs measured by respiratory tests, O2 saturation levels in ambient air, or physical signs and symptoms of respiratory distress. They are organized into four main groups: adrenergic/sympathomimetics, methylxanthines, corticosteroids and anticholinergics.
- Adrenergic and Sympathomimetics: Are compounds that stimulate and mimic the effects of endogenous agonists of the sympathetic nervous system.
- Methylxanthines: Derived from purine, have both bronchodilatory and stimulatory effects.
- Corticosteroids: Are mostly used for anti-inflammatory effects and are a synthetic version of hormones that are usually produced by the adrenal glands.
- Anticholinergics: Block the action of acetylcholine, a neurotransmitter.
In addition to the therapies already mentioned, we have combined products; these usually involve a two-bronchodilator combination, and the delivery mechanism is inhalation. The most common formulas include fluticasone + salmeterol, ipratropium + albuterol, and budesonide + formoterol.
Table 2
Bronchodilators
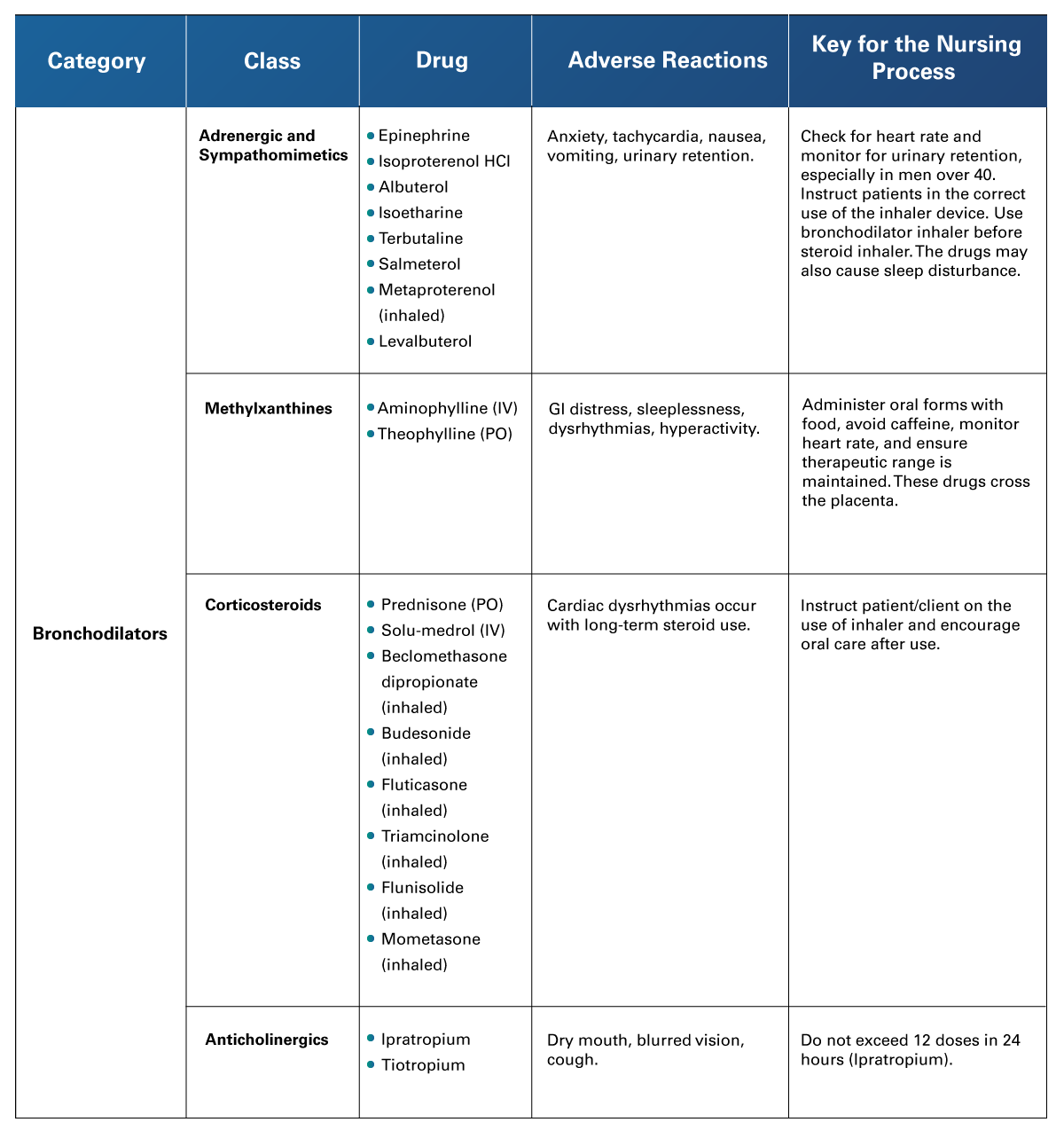 Adapted from Cleveland Clinic. (n. d.). Beers Criteria. https://my.clevelandclinic.org/health/articles/24946-beers-criteria; Sharma et al. (2023). Asthma Medications. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK531455/
Adapted from Cleveland Clinic. (n. d.). Beers Criteria. https://my.clevelandclinic.org/health/articles/24946-beers-criteria; Sharma et al. (2023). Asthma Medications. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK531455/
2.2 Endocrine and Reproductive System
 There has been universal consensus over the last few years on the effective management of diabetes mellitus. Experts and guidelines concur that the disease requires an approach with an interprofessional perspective involving both lifestyle modifications like diet and exercise in combination with pharmacologic therapies as needed to meet individualized glycemic goals in each patient.
There has been universal consensus over the last few years on the effective management of diabetes mellitus. Experts and guidelines concur that the disease requires an approach with an interprofessional perspective involving both lifestyle modifications like diet and exercise in combination with pharmacologic therapies as needed to meet individualized glycemic goals in each patient.
For optimal glycemic control, patients must combine lifestyle changes with oral pharmacologic agents, especially as type 2 diabetes mellitus progresses with continued loss of pancreatic beta-cell function and insulin production (Bhalla et al., 2020).
Healthcare providers should aim for therapies that consistently achieve glycemic control and fulfill educational goals for diabetes management (Bhalla et al., 2020).
These medications are organized in seven groups: sulfonylureas, meglitinides, biguanides, thiazolidinediones, alpha-glucosidase inhibitors, DDP-4 inhibitors and the various insulins. Another important function of endocrine pharmaceuticals is contraception, which is based on hormonal therapy.
- Sulfonylureas: They function by attaching to potassium channels sensitive to adenosine triphosphate (K-ATP channels) located in the pancreas's beta cells. This leads to lowering blood sugar by stimulating the release of insulin by b-cells. Differences between first and second generation are that the first gen is low potency and short acting, and the second gen is high potency and long acting.
- Meglitinides: They lower blood sugar by stimulating b-cells in the pancreas to release insulin. This is achieved by closing K+ channels, which increases insulin secretion.
- Biguanides: They enhance the activity of the enzyme adenosine monophosphate-activated protein kinase, reducing hepatic gluconeogenesis and lipogenesis to increase insulin-mediated uptake of glucose in the muscles. In simpler words: they inhibit hepatic glucose production by increasing peripheral tissue sensitivity to insulin.
- Thiazolidinediones: They reduce blood sugar levels by diminishing tissue resistance to insulin. Consequently, this leads to enhanced glucose absorption in the periphery and elevates adiponectin levels, a cytokine secreted by fat tissue. This not only increases the number of insulin-sensitive adipocytes but also encourages the oxidation of fatty acids (Bhalla et al., 2020).
- Alpha-glucosidase Inhibitors: They lower blood glucose by blunting sugar levels after meals. This inhibits polysaccharide reabsorption and the metabolism of sucrose to glucose and fructose.
- DDP-4 Inhibitors: Lower blood sugar by preventing the degradation of incretins which, in turn, increases insulin secretion.
- Insulins: their analogs were first introduced in 1996. Ever since insulin therapy options for patients with type 1 and type 2 diabetes have expanded enabling insulin therapies to more closely mimic physiological insulin secretion by the pancreas and therefore achieving better glycemic control in patients with diabetes (Liu & Yang, 2019).
- Contraceptive Medication: All oral contraceptives are hormone based. Estrogen pills may prevent the pituitary secretion of FSH, thus inhibiting the ovulation process, although menstruation still occurs. Oral contraceptives have the lowest failure rates of all methods, contributing to their popularity.
Table 3
Endocrine Medication
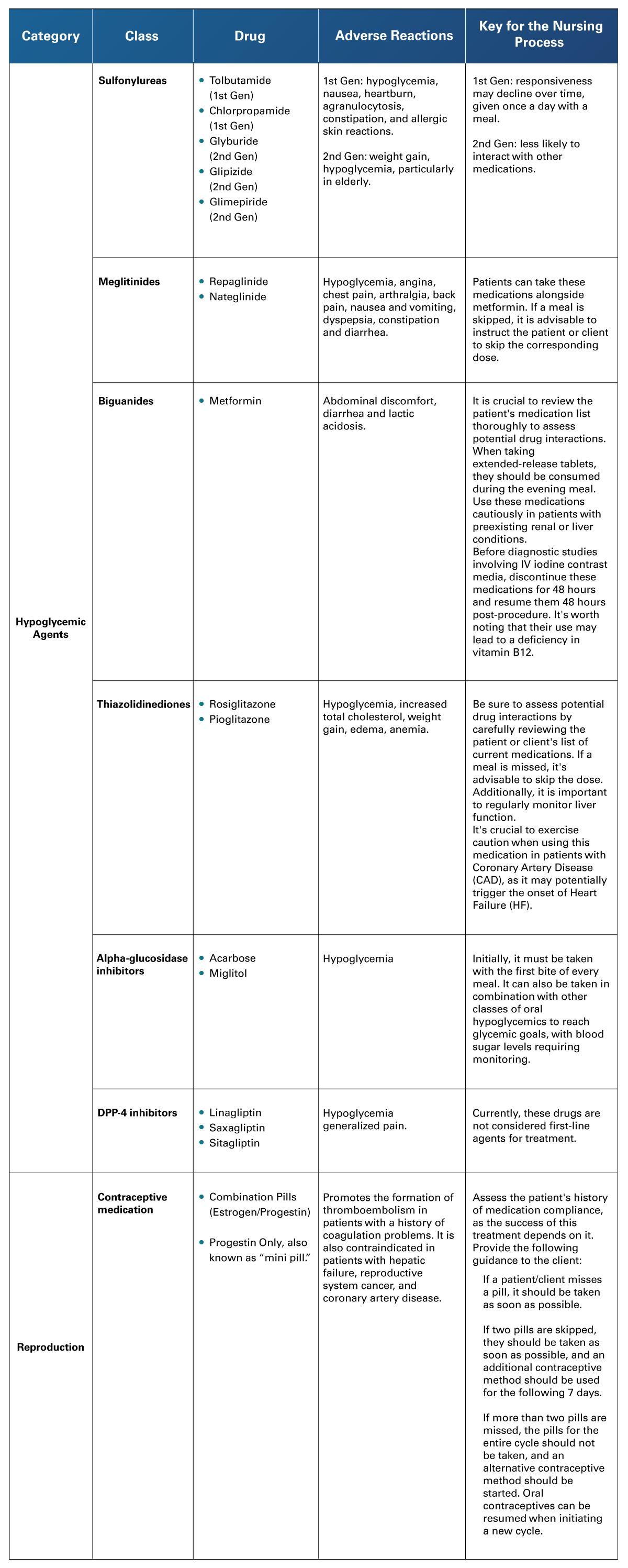 Adapted from Bhalla et al. (2020). Contemporary Meta-Analysis of Extended Direct-Acting Oral Anticoagulant Thromboprophylaxis to Prevent Venous Thromboembolism. Am J Med. http://doi.org/10.1016/j.amjmed.2020.01.037; Colbert, B., & Woodrow, R. (2017). Essentials of Pharmacology for Health Professions. Cengage Learning.
Adapted from Bhalla et al. (2020). Contemporary Meta-Analysis of Extended Direct-Acting Oral Anticoagulant Thromboprophylaxis to Prevent Venous Thromboembolism. Am J Med. http://doi.org/10.1016/j.amjmed.2020.01.037; Colbert, B., & Woodrow, R. (2017). Essentials of Pharmacology for Health Professions. Cengage Learning.
Table 4
Types of Insulins
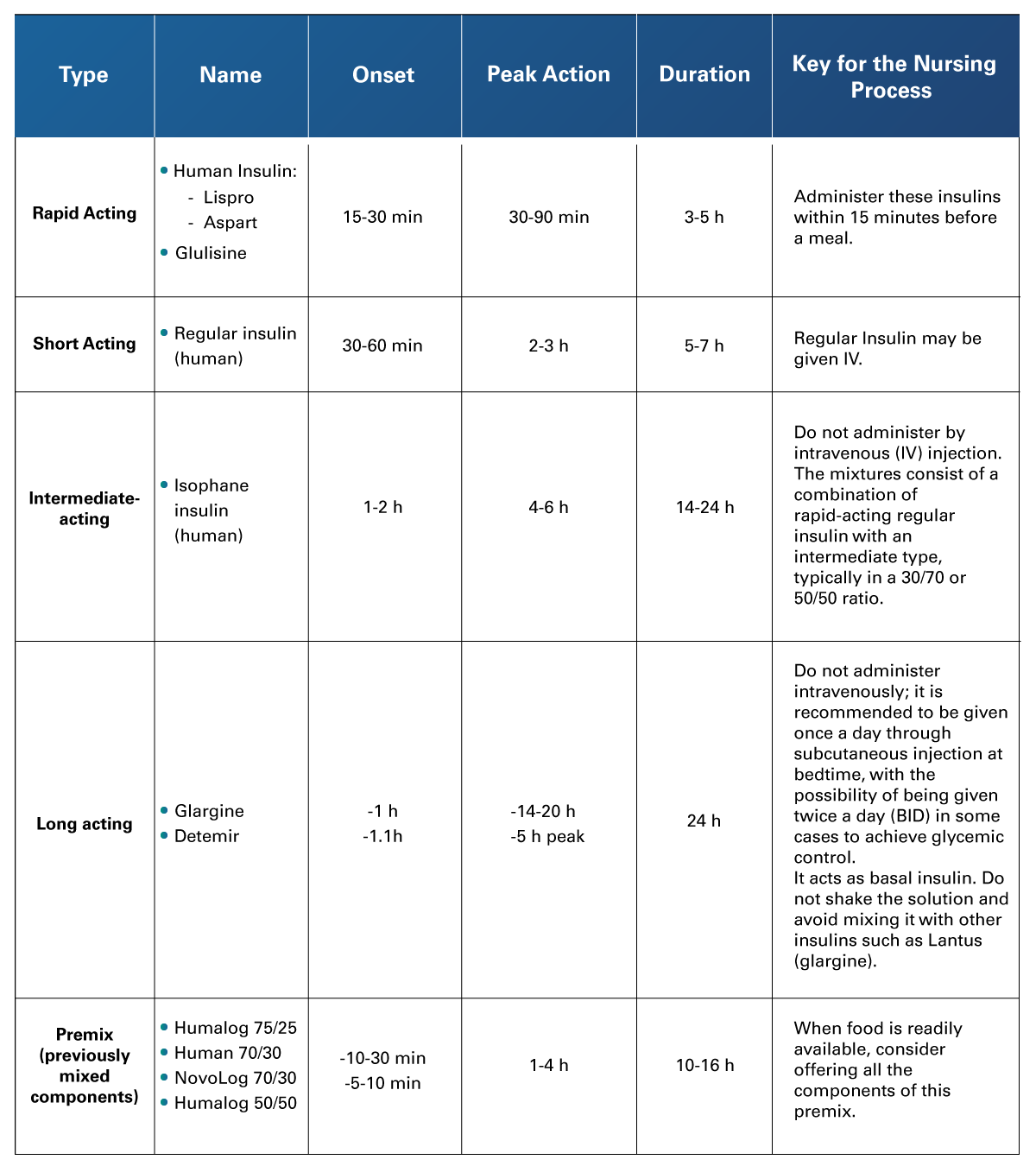 Adapted from Colbert, B., & Woodrow, R. (2017). Essentials of Pharmacology for Health Professions. Cengage Learning; Liu, Z., & Yang, B. (2019). Curr Drug Targets, 20(8). http://doi.org/10.2174/1389450120666181217111500
Adapted from Colbert, B., & Woodrow, R. (2017). Essentials of Pharmacology for Health Professions. Cengage Learning; Liu, Z., & Yang, B. (2019). Curr Drug Targets, 20(8). http://doi.org/10.2174/1389450120666181217111500
2.3 Gastrointestinal System
 Gastrointestinal drugs are popular among patients given the fact that many of them are easy to acquire without a prescription, the most common ones being antiulcer and antiemetic drugs. The first group works by neutralizing or reducing acidity of stomach contents, and are organized into four main groups: antiacids, H2-receptor antagonists, mucosal protectants and proton pump inhibitors. Antiemetics work to prevent the patient from nausea and vomiting. In the traditional healthcare setting nausea may be one of the most common symptoms encountered, given the nature of the symptom itself is also amongst patients' main complaints while being taken to the emergency room. The origins of nausea range from a bodily defense against toxins to a nuanced blend of triggers such as stress, medication, or even fear. Different neurohumoral pathways might be implicated. (Michaels et al., 2018). These medications are organized in groups: serotonin-receptor antagonists, glucocorticoids, anticholinergics, benzamides and antihistamines.
Gastrointestinal drugs are popular among patients given the fact that many of them are easy to acquire without a prescription, the most common ones being antiulcer and antiemetic drugs. The first group works by neutralizing or reducing acidity of stomach contents, and are organized into four main groups: antiacids, H2-receptor antagonists, mucosal protectants and proton pump inhibitors. Antiemetics work to prevent the patient from nausea and vomiting. In the traditional healthcare setting nausea may be one of the most common symptoms encountered, given the nature of the symptom itself is also amongst patients' main complaints while being taken to the emergency room. The origins of nausea range from a bodily defense against toxins to a nuanced blend of triggers such as stress, medication, or even fear. Different neurohumoral pathways might be implicated. (Michaels et al., 2018). These medications are organized in groups: serotonin-receptor antagonists, glucocorticoids, anticholinergics, benzamides and antihistamines.
- Antiacids: Relieve heartburn and indigestion by reducing the amount of acid production in the stomach.
- H2-receptor Antagonists: Widely used in the treatment of acid-peptic disease, gastric and duodenal ulcers, gastroesophageal reflux disease and heartburn. The 4 types of this drugs that are currently in use are widely available either by prescription or over-the-counter, and are some of the most widely used in allopathic medicine. They work by way of the H2 receptor blockers binding to histamine type 2 receptors on the basolateral (antiluminal) surface of gastric parietal cells (responsible for gastric acid secretion), interfering with pathways of gastric acid production and secretion.
- Mucosal Protectants: Frequently used in the treatment of peptic ulcers to aid with mucosal repair secondary to damage sustained for long periods of time.
- Proton Pump Inhibitors: Class of drugs that are widely known for their popular use in acid-related conditions. Omeprazole alone is listed as one of the top 10 most prescribed drugs in the United States. They are often chosen as the first-line agents amongst gastroenterologists for the treatment of esophagitis, non-erosive reflux disease, peptic ulcer disease, prevention of ulcers induced by NSAIDs, Zollinger-Ellison syndrome and as part of the triple therapy regimen for Helicobacter pylori infections.
- Serotonin-receptor Antagonists: These work by blocking serotonin from interacting with the 5-HT3 receptor. Of these groups, ondansetron and granisetron are the most frequently used/prescribed.
- Glucocorticoids: Their mechanism of action is not clearly understood. Dexamethasone is widely used and studied as complementary therapy with chemotherapy and in the prevention of postoperative nausea and vomiting, as the literature indicates.
- Anticholinergics: Scopolamine is the most commonly prescribed/used drug of this class. It is mostly used to treat motion sickness or as a prophylactic in the perioperative setting.
- Benzamides: Antagonize the D2 receptor when administered in low doses but can also antagonize the 5-HT3 receptor when given at higher doses.
- Antihistamines: Typically used to treat symptoms of allergic reactions. They are widely used as promotility agents. These drugs antagonize both histamine H1 and H2 receptors.
Table 5
Gastrointestinal Medications
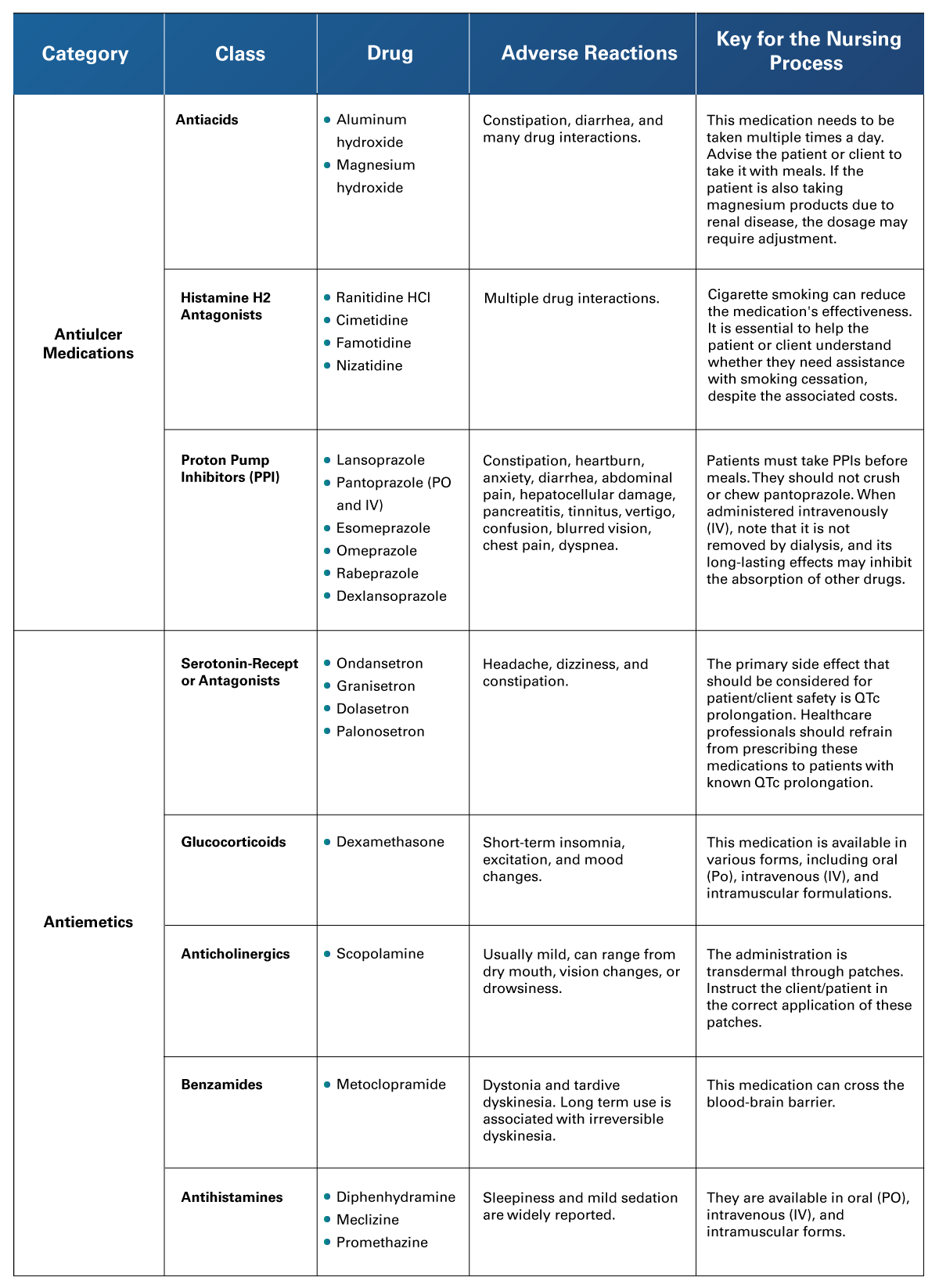 Adapted from Colbert, B., & Woodrow, R. (2017). Essentials of Pharmacology for Health Professions. Cengage Learning; Michels et al. (2018). Modification of the Associations Between Duration of Oral Contraceptive Use and Ovarian, Endometrial, Breast, and Colorectal Cancers. JAMA Oncology, 4(4). https://doi.org/10.1001/jamaoncol.2017.4942
Adapted from Colbert, B., & Woodrow, R. (2017). Essentials of Pharmacology for Health Professions. Cengage Learning; Michels et al. (2018). Modification of the Associations Between Duration of Oral Contraceptive Use and Ovarian, Endometrial, Breast, and Colorectal Cancers. JAMA Oncology, 4(4). https://doi.org/10.1001/jamaoncol.2017.4942
2.4 Hematologic and Immune System
 A serious risk in the hematologic system is the formation of thrombus. Antithrombotic drugs include anticoagulants and antiplatelets. Irregularities in the blood vessel wall and clotting elements lead to the transformation of liquid fibrinogen into solid fibrin, causing clotting. Various anticoagulant choices are available, and medical professionals determine the appropriate one based on its intended use, patient's choice, the effectiveness of anticoagulants in certain clinical scenarios, and established treatment recommendations.
A serious risk in the hematologic system is the formation of thrombus. Antithrombotic drugs include anticoagulants and antiplatelets. Irregularities in the blood vessel wall and clotting elements lead to the transformation of liquid fibrinogen into solid fibrin, causing clotting. Various anticoagulant choices are available, and medical professionals determine the appropriate one based on its intended use, patient's choice, the effectiveness of anticoagulants in certain clinical scenarios, and established treatment recommendations.
There are several conditions in which anticoagulation should be avoided, the nurse needs to inform the MD if the patient/client has one of the following: active bleeding, gastrointestinal bleeding, coagulopathy, recent major surgeries, acute intracranial hemorrhage, major trauma, aortic dissection or aneurysm, and the geriatric or pregnant patients.
Anticoagulants are organized in groups: heparin, warfarin, factor Xa inhibitor and New Oral Anticoagulants (NOAC). Antiplatelets are organized in antiplatelet agents, low molecular weight heparins and group IIa-IIb inhibitors.
- Heparin Sodium: An antagonist to thrombin and works by way of preventing the conversion of fibrinogen to fibrin.
- Low Molecular Weight Heparins: Used in the prevention of thrombus formation leading to DVT (Deep Vein Thrombosis). Widely used in the surgical and orthopedic fields.
- Warfarin Sodium: Blocks the formation of prothrombin from vitamin K.
- Factor Xa Inhibitor: Used in the prevention of thrombus formation leading to DVT. Widely used in the surgical and orthopedic fields.
- New Oral Anticoagulants (NOAC): Indicated for DVT prevention in orthopedic surgery, prevention of stroke and systemic embolism and patients with atrial fibrillation. They specifically inhibit factors 2a (thrombin) or 10a.
- Antiplatelet Agents: Preferred for short-term use after cardiac interventions, they reduce the risk for thrombolytic stroke in those who are intolerant to aspirin. Preventive in thrombolytic disorders.
- Group IIa/IIb Inhibitors: Inhibitors like tirofiban and eptifibatide, which target glycoprotein IIb/IIIa, are solely accessible in parenteral form and are utilized during the intense stages of acute coronary syndrome.
Table 6
Hematologic Medications
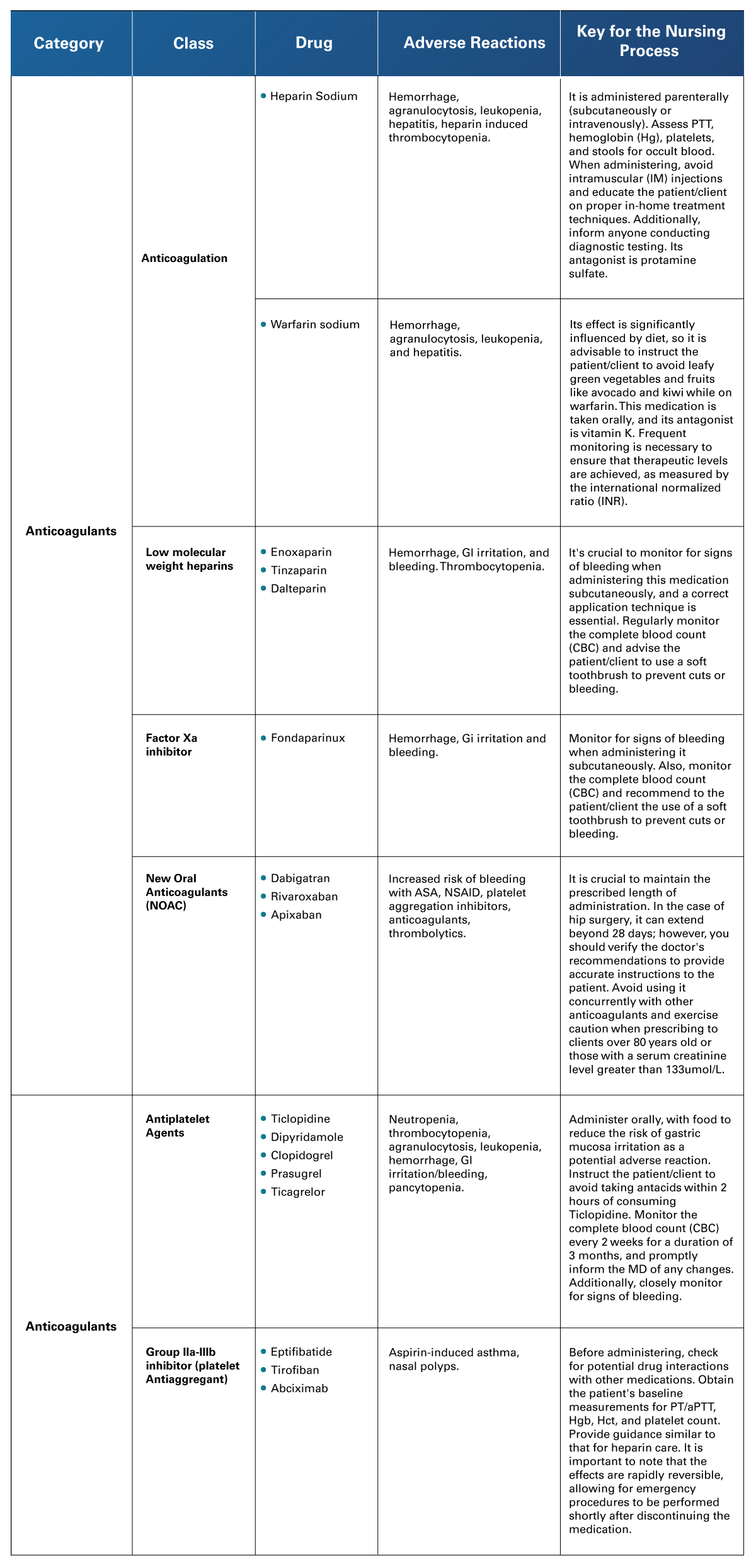 Adapted from Bhalla et al. (2020). Contemporary Meta-Analysis of Extended Direct-Acting Oral Anticoagulant Thromboprophylaxis to Prevent Venous Thromboembolism. Am J Med. http://doi.org/10.1016/j.amjmed.2020.01.037; Colbert, B., & Woodrow, R. (2017). Essentials of Pharmacology for Health Professions. Cengage Learning; Schug et al. (2020). Acute Pain Management: Scientific Evidence. Australian and New Zealand College of Anesthetists and Faculty of Pain Medicine. https://www.anzca.edu.au/resources/college-publications/acute-pain-management/apmse5.pdf; Su et al. (2020). Meta-analysis of the Efficacy and Safety of Non-vitamin K Antagonist Oral Anticoagulants with Warfarin in Latin American Patients with Atrial Fibrillation. Medicine. https://doi.org/10.1097/MD.0000000000019542
Adapted from Bhalla et al. (2020). Contemporary Meta-Analysis of Extended Direct-Acting Oral Anticoagulant Thromboprophylaxis to Prevent Venous Thromboembolism. Am J Med. http://doi.org/10.1016/j.amjmed.2020.01.037; Colbert, B., & Woodrow, R. (2017). Essentials of Pharmacology for Health Professions. Cengage Learning; Schug et al. (2020). Acute Pain Management: Scientific Evidence. Australian and New Zealand College of Anesthetists and Faculty of Pain Medicine. https://www.anzca.edu.au/resources/college-publications/acute-pain-management/apmse5.pdf; Su et al. (2020). Meta-analysis of the Efficacy and Safety of Non-vitamin K Antagonist Oral Anticoagulants with Warfarin in Latin American Patients with Atrial Fibrillation. Medicine. https://doi.org/10.1097/MD.0000000000019542
2.5 Musculoskeletal, neurologic and pain management
 In this group of medications, there is a broad variety of drugs, from over-the-counter PO administered compounds to intricately delivered IV pump drugs. They also provide solutions for some of the most common symptoms in various medical contexts, including emergency rooms and medical-surgical floors. Analgesics may be administered via the following routes: oral, intramuscular, rectal, IV bolus (push), continuous subcutaneous narcotic infusion, continuous epidural analgesia, transdermal patches, or patient-controlled analgesia. Major analgesic groups are nonsteroidal anti-inflammatory drugs and opioids.
In this group of medications, there is a broad variety of drugs, from over-the-counter PO administered compounds to intricately delivered IV pump drugs. They also provide solutions for some of the most common symptoms in various medical contexts, including emergency rooms and medical-surgical floors. Analgesics may be administered via the following routes: oral, intramuscular, rectal, IV bolus (push), continuous subcutaneous narcotic infusion, continuous epidural analgesia, transdermal patches, or patient-controlled analgesia. Major analgesic groups are nonsteroidal anti-inflammatory drugs and opioids.
- Nonsteroidal Anti-inflammatory Drugs: A very popular group of drugs known for their antipyretic, analgesic, and anti-inflammatory properties. Most of them are available in several forms and routes of administration with many available as over-the-counter medications.
- Opioids: As adjuncts to other analgesics in pain management, they are well known for enhancing the effects of other analgesic therapies and are widely used in surgery, such as postoperative pain management, and in the oncology setting.
Table 7
Musculoskeletal, Neurologic and Pain Management Medications
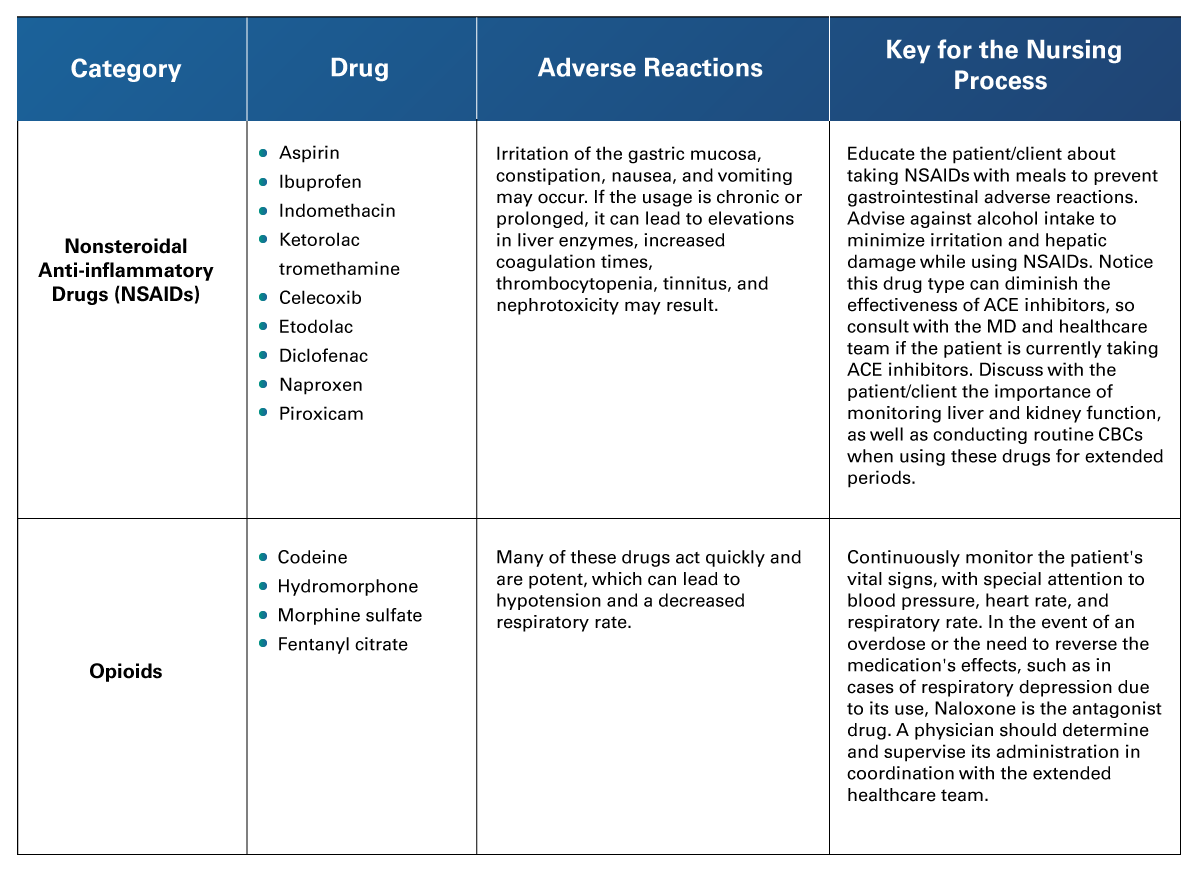 Adapted from Cohen et al. (2023). Opioid Analgesics. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459161/; Ghlichloo, I., & Gerriets, V. (2023). Nonsteroidal Anti-Inflammatory Drugs (NSAIDs). StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK547742/; Schug et al. (2020). Acute Pain Management: Scientific Evidence. Australian and New Zealand College of Anesthetists and Faculty of Pain Medicine. https://www.anzca.edu.au/resources/college-publications/acute-pain-management/apmse5.pdf
Adapted from Cohen et al. (2023). Opioid Analgesics. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459161/; Ghlichloo, I., & Gerriets, V. (2023). Nonsteroidal Anti-Inflammatory Drugs (NSAIDs). StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK547742/; Schug et al. (2020). Acute Pain Management: Scientific Evidence. Australian and New Zealand College of Anesthetists and Faculty of Pain Medicine. https://www.anzca.edu.au/resources/college-publications/acute-pain-management/apmse5.pdf
2.6 Infectious diseases
 Since Alexander Fleming’s discovery of Penicillin in 1928, allopathic medicine has come to rely heavily on anti-infective drugs for treating infections and preventing them in surgical settings or in patients with a compromised immune system. The following table shows the different families within these drugs, indications, adverse reactions and most importantly the Key to the Nursing Process which considers the best practices for nurses to adopt while treating and educating a client/patient. Modern antibiotics are organized in groups: penicillin, antipseudomonal penicillin (and combinations), semisynthetic, tetracyclines, aminoglycosides, cephalosporins, carbapenems, monobactam, macrolides, fluoroquinolones, lacosamide, streptogramin, and oxazolidinone.
Since Alexander Fleming’s discovery of Penicillin in 1928, allopathic medicine has come to rely heavily on anti-infective drugs for treating infections and preventing them in surgical settings or in patients with a compromised immune system. The following table shows the different families within these drugs, indications, adverse reactions and most importantly the Key to the Nursing Process which considers the best practices for nurses to adopt while treating and educating a client/patient. Modern antibiotics are organized in groups: penicillin, antipseudomonal penicillin (and combinations), semisynthetic, tetracyclines, aminoglycosides, cephalosporins, carbapenems, monobactam, macrolides, fluoroquinolones, lacosamide, streptogramin, and oxazolidinone.
- Penicillin: Belongs to the beta-lactam antibiotic class. They have a wide range of clinical applications: from gram-positive cocci and rods to most anaerobes.
- Antipseudomonal Penicillin: Has most of the activity against bacteria that penicillin and aminopenicillins have. They are also effective against gram-negative rods.
- Semisynthetic Penicillin: Provides improved activity against a broad range of organisms, including streptococcus, staphylococcus, aerobic gram-negative organisms, and most anaerobes.
- Tetracyclines: Used against infections of the respiratory tract, skin, urinary, genital and intestinal systems. Also, for infections spread by ticks, lice and other infected animals.
- Aminoglycosides: Natural or semisynthetic antibiotics derived from actinomycetes. They work together with many other antibacterial classes.
- Cephalosporins: Beta-lactam antimicrobials used against gram-positive and gram-negative bacteria.
- Carbapenems: They have the broadest spectrum of activity and highest potency against gram-positive and gram-negative bacteria. Considered as the last-line agents because of this.
- Monobactam: Synthetic compounds, beta-lactam antibiotics. They exhibit cross-activity with cephalosporins.
- Macrolides: Derived from Saccharopolyspora erythraea, a bacterium naturally found in soil. They are potent inhibitors of protein synthesis.
- Fluoroquinolones: Synthetic, broad spectrum, systemic antibiotics. Mostly used for respiratory and urinary tract infections.
- Lincosamides: Mostly known as the alternative used for patients allergic to penicillin.
- Streptogramin: Cyclic peptide antibiotics that inhibit the synthesis of bacterial proteins.
- Oxazolidinone: The newest group of antibiotics. They are synthetic and have a broad spectrum of activity against gram-positive bacteria, including those that are resistant to other antibiotics.
Table 8
Antibiotics
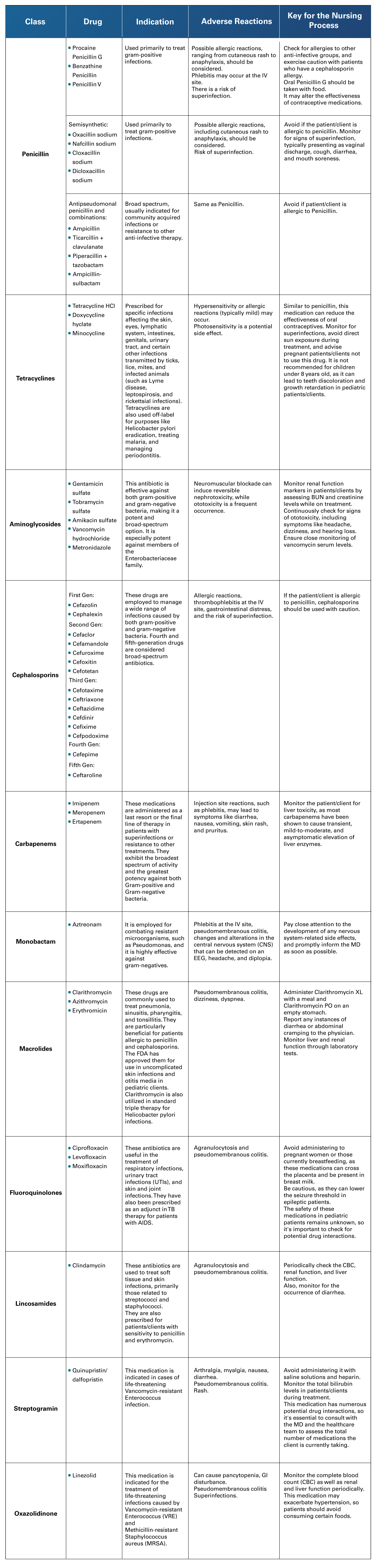 Adapted from Moore, L. S. P., & Hatcher, J.C. (2020). Infectious Diseases: Microbiology and Virology. Cambridge University Press.
Adapted from Moore, L. S. P., & Hatcher, J.C. (2020). Infectious Diseases: Microbiology and Virology. Cambridge University Press.
 The pharmacology of systems can be a daunting subject given that in modern medicine there is a wide selection of drugs that may target the same disease. For a better understanding, it is vital for the nurse to grasp the mechanisms of action, adverse reactions, and, especially, all the information contained in the Key for The Nursing Process. It is essential for the nursing professional to instruct patients/clients on the use of and precautions necessary for reaching therapeutic goals with their pharmacologic treatments.
The pharmacology of systems can be a daunting subject given that in modern medicine there is a wide selection of drugs that may target the same disease. For a better understanding, it is vital for the nurse to grasp the mechanisms of action, adverse reactions, and, especially, all the information contained in the Key for The Nursing Process. It is essential for the nursing professional to instruct patients/clients on the use of and precautions necessary for reaching therapeutic goals with their pharmacologic treatments.
At the same time, the nurse should also be aware of interactions and contraindications of a given drug and correlate this information with the patient's/client's overall condition. Are these the best treatment choices considering the patient’s individual and social context, support system, level of understanding, and ability to comply with medication?
As a leader and advocate for the patient, the nurse should also raise awareness within the treatment team if the drug of choice may not be the best option, considering the aforementioned issues.
- Bhalla, V., Lamping, O. F., Abdel-Latif, A., Bhalla, M., Ziada, K., & Smyth, S.S. (2020). Contemporary Meta-Analysis of Extended Direct-Acting Oral Anticoagulant Thromboprophylaxis to Prevent Venous Thromboembolism. Am J Med. http://doi.org/10.1016/j.amjmed.2020.01.037
- Cleveland Clinic. (n. d.). Beers Criteria. https://my.clevelandclinic.org/health/articles/24946-beers-criteria
- Colbert, B., & Woodrow, R. (2017). Essentials of Pharmacology for Health Professions (8th ed.). Cengage Learning.
- Ghlichloo, I., & Gerriets, V. (2023, January). Nonsteroidal Anti-Inflammatory Drugs (NSAIDs). StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK547742/
- Liu, Z., & Yang, B. (2019). Drug Development Strategy for Type 2 Diabetes: Targeting Positive Energy Balances. Curr Drug Targets, 20(8), 879-890. http://doi.org/10.2174/1389450120666181217111500
- Michels, K. A., Pfeiffer, R. M., Brinton, L. A., & Trabert, B. (2018). Modification of the associations between duration of oral contraceptive use and ovarian, endometrial, breast, and colorectal cancers. JAMA Oncology, 4(4), 516–521. https://doi.org/10.1001/jamaoncol.2017.4942
- Moore, L. S. P., & Hatcher, J.C. (2020). Infectious Diseases: Microbiology and Virology (1st ed.). Cambridge University Press.
- Schug, S. A., Palmer, G. M., Scott, D. A., Alcok, M., Halliwell, R., & Mott, J. (2020). Acute Pain Management: Scientific Evidence (5th ed.). Australian and New Zealand College of Anesthetists and Faculty of Pain Medicine. https://www.anzca.edu.au/resources/college-publications/acute-pain-management/apmse5.pdf
- Sharma, S., Hashmi, M. F., & Chakraborty, R. K. (2023, June 20). Asthma Medications. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK531455/
- Spechler, S. J. (2019, January). Proton Pump Inhibitors: What the Internist Needs to Know. Med Clin North Am. https://pubmed.ncbi.nlm.nih.gov/30466666/
- Su, Z., Zhang, H., He, W., Ma, J., Zeng, J., & Jiang, X. (2020). Meta-analysis of the efficacy and safety of non-vitamin K antagonist oral anticoagulants with warfarin in Latin American patients with atrial fibrillation. Medicine. https://doi.org/10.1097/MD.0000000000019542
The following links do not belong to Tecmilenio University, when accessing to them, you must accept their terms and conditions.
Readings
- American Heart Association. (2022, November 17). A Patient’s Guide to Taking Warfarin. https://www.heart.org/en/health-topics/arrhythmia/prevention--treatment-of-arrhythmia/a-patients-guide-to-taking-warfarin
- Elsevier. (2023, July 25). Blood, Glucose Monitoring, Adults. https://elsevier.health/en-US/preview/blood-glucose-monitoring-adult
Videos
- AJMC Peer Exchange. (2023, January 4). Patient Education and Proper Inhaler Technique [Video]. AJMC. https://www.ajmc.com/view/patient-education-and-proper-inhaler-technique
- Shuwarger, M. (2021, August, 25). Maternity – Preconception, part 2: Hormonal Methods of Contraception [Video]. Level UP RN. https://www.leveluprn.com/blogs/maternity-nursing/preconception-2-hormonal-methods-contraception
La obra presentada es propiedad de ENSEÑANZA E INVESTIGACIÓN SUPERIOR A.C. (UNIVERSIDAD TECMILENIO), protegida por la Ley Federal de Derecho de Autor; la alteración o deformación de una obra, así como su reproducción, exhibición o ejecución pública sin el consentimiento de su autor y titular de los derechos correspondientes es constitutivo de un delito tipificado en la Ley Federal de Derechos de Autor, así como en las Leyes Internacionales de Derecho de Autor.
El uso de imágenes, fragmentos de videos, fragmentos de eventos culturales, programas y demás material que sea objeto de protección de los derechos de autor, es exclusivamente para fines educativos e informativos, y cualquier uso distinto como el lucro, reproducción, edición o modificación, será perseguido y sancionado por UNIVERSIDAD TECMILENIO.
Queda prohibido copiar, reproducir, distribuir, publicar, transmitir, difundir, o en cualquier modo explotar cualquier parte de esta obra sin la autorización previa por escrito de UNIVERSIDAD TECMILENIO. Sin embargo, usted podrá bajar material a su computadora personal para uso exclusivamente personal o educacional y no comercial limitado a una copia por página. No se podrá remover o alterar de la copia ninguna leyenda de Derechos de Autor o la que manifieste la autoría del material.