Reduction of Risk Potencial / 05
Make sure to:
- Identify errors in medication.
- Describe measures to improve the medication process.
- Understand the importance of medication reconciliation.
 An estimated 7,000 to 9,000 people are believed to die annually in the United States due to medication errors. Apart from the consequential economic cost of $40 million dollars, patients involved in such situations may endure physical or psychological discomfort and face a potential risk of serious complications. Additionally, it is observed that these incidents contribute to dissatisfaction and mistrust in the healthcare system (Tariaq et al., 2023).
An estimated 7,000 to 9,000 people are believed to die annually in the United States due to medication errors. Apart from the consequential economic cost of $40 million dollars, patients involved in such situations may endure physical or psychological discomfort and face a potential risk of serious complications. Additionally, it is observed that these incidents contribute to dissatisfaction and mistrust in the healthcare system (Tariaq et al., 2023).
In this context, the World Health Organization introduced the Medication without Harm initiative (World Health Organization, 2022) with the goal of improving the medication process. Previously, during the 72nd Assembly in 2019, World Patient Safety Day was established. According to Jonás Gonseth García, a Quality Consultant at the Pan American Health Association, it is acknowledged that "most medication errors are associated with confusion between drugs with similar names, errors in dosage or routes of administration, and failures to reconcile the new medication with what the patient is already taking” (Pan American Health Association, 2022).
It is crucial to emphasize that the training of healthcare personnel regarding the prescription, storage, transcription, preparation, and administration of medications is essential for preventing medication errors. Additionally, involving the patient in their treatment by educating them about the effects of medications is important. This empowers them to report any adverse effects promptly and communicate them to the physician or nurse in a timely manner.
2.1 Administration and Monitoring
 According to Le (2022), a drug is defined by U.S. law as “any substance (other than a food or device) used for the diagnosis, treatment, cure, or prevention of disease, or to treat conditions affecting the structure or functioning of the body”. For a drug to fulfill its intended purpose, it must meet therapeutic criteria in terms of dosage, frequency, and route of administration.
According to Le (2022), a drug is defined by U.S. law as “any substance (other than a food or device) used for the diagnosis, treatment, cure, or prevention of disease, or to treat conditions affecting the structure or functioning of the body”. For a drug to fulfill its intended purpose, it must meet therapeutic criteria in terms of dosage, frequency, and route of administration.
Patient responses to drugs vary due to individual factors, including age, body size, consumption of other drugs and dietary supplements, food, presence of renal or hepatic disease, development of tolerance and resistance, and their adherence to the treatment. At the extremes of life, liver and kidney function are less effective, leading to the accumulation of medications in the system. Additionally, older adults often present with multiple chronic conditions, necessitating multiple and simultaneous treatments, which poses risks of drug interactions.
According to Hughe (2008), a crucial pillar in patient medication is the nurse, who may encounter various circumstances that contribute to medication errors. These situations include colleagues with inadequate training in patient safety and quality, excessive workload, insufficient staffing, fatigue, illegible provider handwriting, faulty dispensing systems, and issues with medication labeling. Despite these challenges, nurses are consistently tasked with ensuring that their patients receive the right medication at the right time.
The three primary routes for drug administration are enteral, topical and parenteral.
The enteral route encompasses drugs administered orally and those delivered through a nasogastric or gastrostomy tube.
Table 1
Primary Routes for Drug Administration
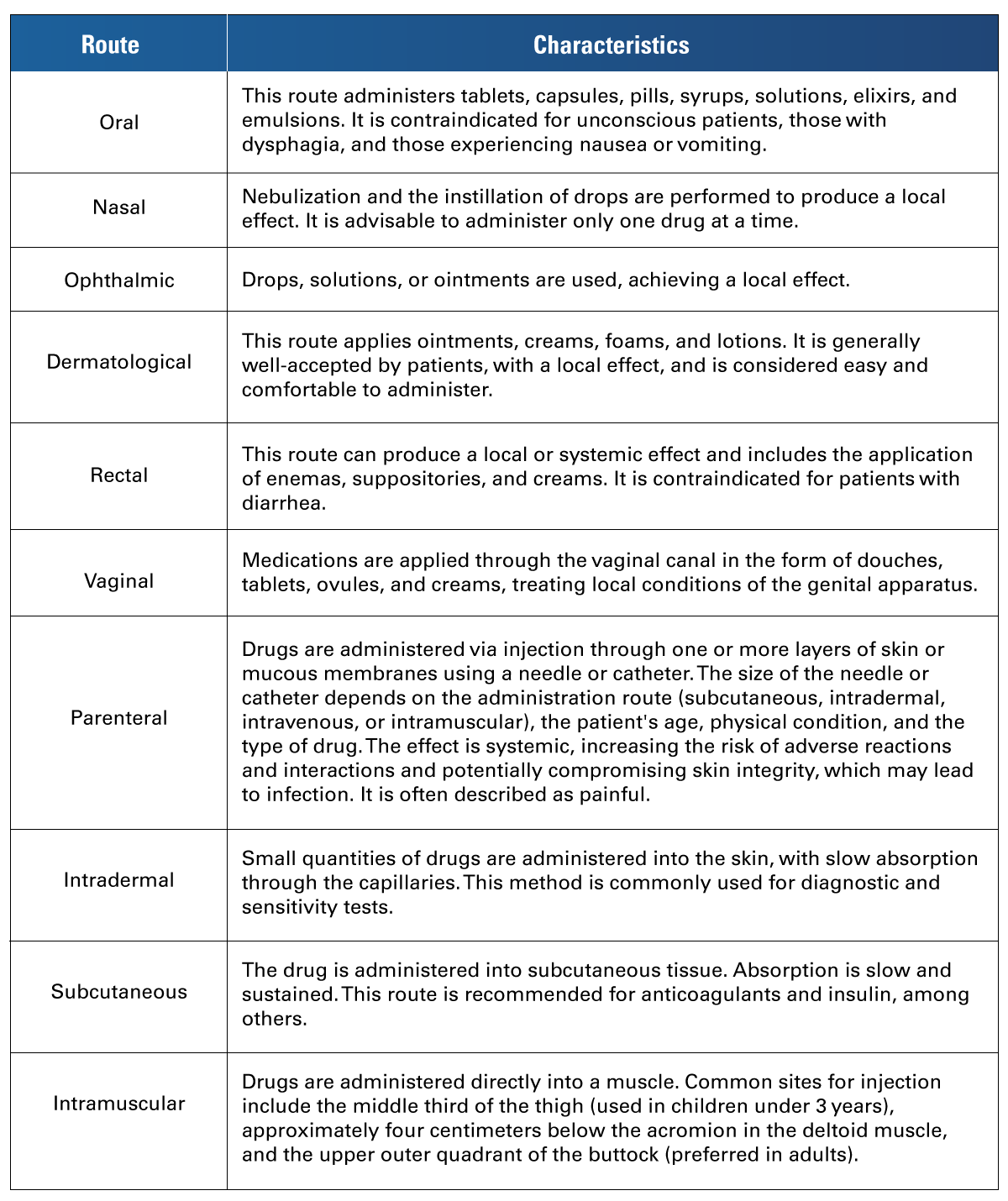 Adapted from Pinargote-Chancay et al. (2018). Fundamentos Teóricos y Prácticos de Enfermería. Mawil Publicaciones Impresas y Digitales. https://mawil.us/wp-content/uploads/2021/04/fundamentos-teoricos-y-practicos-de-enfermeria.pdf
Adapted from Pinargote-Chancay et al. (2018). Fundamentos Teóricos y Prácticos de Enfermería. Mawil Publicaciones Impresas y Digitales. https://mawil.us/wp-content/uploads/2021/04/fundamentos-teoricos-y-practicos-de-enfermeria.pdf
Considerations for safe preparation and administration (Pinargote-Chancay et al., 2018):
- Maintain a high degree of focus throughout the process.
- Visualize the commercial name, active ingredient, and expiration date on the medicine.
- Avoid wetting the label of the bottles.
- Place tablets, pills, or capsules on a glass surface for treatment.
- Never administer medicines prepared by other professionals.
- Once the medications have been prepared, do not return them to the container.
- When preparing and administering parenteral drugs, use sterile technique.
- Use the diluents recommended on the label.
- Check the concentration (amount of diluent recommended) and speed of administration (slow, moderate, or fast).
- Dispose of needles and other materials according to biosafety measures.
The International Patient Safety Goals (IPSG) proposed by the Joint Commission directly impact medication management. IPSG 1 mandates correct patient identification before administering medication. The patient's identity must be verified before proceeding with the procedure. As for IPSG 2, it emphasizes effective communication, both orally and in writing. The prescriber should maintain legible handwriting, avoid abbreviations, and consider decimal point values. The person receiving the written prescription should read it aloud for the prescriber to confirm. In cases of telephone prescriptions, the recommended process is "Listen-Write-Read-Confirm," where the receiver writes down and reads aloud what they heard, and the sender confirms the accuracy of the prescription. Additionally, IPSG 5, focused on the Prevention of Healthcare-Associated Infections, highlights the importance of handwashing before preparing and administering medications. It underscores the significance of maintaining the sterility of syringes, needles, catheters, solutions, and medications during handling.
According to Hughes (2008), medication error can be describe as a preventable incident that can result in incorrect medication utilization or harm to a patient can occur while the medication is managed by health professionals, patients, or consumers. These incidents can involve various aspects of healthcare services such as prescription writing; communication of orders; labeling, packaging, and naming of products; compound preparation; dispensing; distributing; administering; providing education; monitoring; and the actual consumption of the medication.
Safe medication administration involves, at a minimum, verification considerations for correct medication administration (Lilley et al., 2019).
- Choose the correct medication. Verify the prescription, expiration date, and prescribed presentation.
- Prepare the correct dosage. Check against the prescription. Label each medication or solution as soon as it is prepared, unless it is immediately administered. Whenever a dose seems inadequate, recheck it.
- Administer the medication to the indicated patient. Verify the patient's identity, as established on IPSG 1.
- Administer medication by the correct route. Ensure the route of administration is correct. If the route does not appear on the prescription, consult with the treating physician.
- Administer the medication at the correct time and frequency prescribed. Check the appearance of the drug before administration, detecting any color changes or precipitations.
- Check the infusion rate.
- Record all medications administered. Record and sign the appropriate forms as soon as possible. If a medication is not administered, record the reason. If a medication is administered as needed, record it and note the reason.
- Inform and instruct the patient about the medications administered.
- Confirm that the patient only takes prescribed medications.
- Investigate if the patient is allergic to any drugs.
- Wash hands before preparing and administering medications.
According with The Joint Commission (2023), IPSG 3 concentrates on enhancing the safety of high-risk medications, which include:
- Concentrated Electrolytes
- Chemotherapeutics
- Radiopharmaceuticals
- Insulins
- Parenteral anticoagulants
A frequent drug safety problem is the erroneous preparation and/or administration of concentrated electrolytes. This is related to lack of supervision of new staff, lack of orientation and induction of patient care staff, or a poorly managed emergency.
Some recommendations to avoid errors include:
- Removing concentrated electrolytes from patient care areas.
- Not storing them continuously in these areas, separating them from the rest of the medications.
- Establishing visual alerts, such as color coding, regardless of the commercial presentation.
- Implementing the double verification or double "check" during the processes of preparation and administration of high-risk drugs.
The staff should be trained in proper prescribing practices. Illegible, incomplete, or confusing medication prescriptions can jeopardize patient safety and potentially delay treatment. Therefore, the organization should implement measures to prevent medication errors and near misses associated with illegible prescriptions.
Transcription is the process by which personnel authorized by the organization (prescribers) have their indications written down in another document. For instance, this may involve transferring medical indications to the nursing chart, from a medical prescription to the pharmacotherapeutic profile, or during the updating of indications.
Medication labeling is a crucial practice for reducing the risk of medication errors. Labeling medications should occur immediately after preparation or pouring into different containers. The labeling should include, at a minimum, the following data:
- Patient identification data
- Name of the medication
- Dosage, if applicable
- Concentration, if applicable
- Route, if applicable
- Dilution, if applicable
- Date/time of preparation and expiration, if applicable
Labeling may be omitted only if the drug is administered immediately.
Multidose drugs (for example, xylocaine, heparin, insulin), are those that can be used several times for the same patient or multiple times with different patients. They should be labeled with the date/time of preparation and/or opening, along with their expiration date. This is done to ensure sterility and prevent infections.
Physicians, nurses and other healthcare professionals collaborate to monitor patients' response to drug therapy, assessing the drug's impact on symptoms, blood biometry, renal function, liver function, and detecting adverse drug reactions or other side effects.
The specific follow-up that the nurse can provide to the patient involves verifying the decrease of symptoms as an effect of the drugs, such as pain, vomiting, insomnia, or fever. Medications like warfarin require continued administration to monitor the effect on coagulation factor levels. When administering digoxin, blood tests must also be performed to evaluate the effect and determine if a new medication should be applied. This monitoring or follow-up by the nurse helps detect risk situations in the patient related to the use and interactions of prescribed medications.
Table 2
Error-Prone Medication Processes
 Adapted from Hughes, R. G. (2008). Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality. https://www.ncbi.nlm.nih.gov/books/NBK2651/
Adapted from Hughes, R. G. (2008). Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality. https://www.ncbi.nlm.nih.gov/books/NBK2651/
2.2 Polypharmacy
 The Joint Commission (2023) and the World Health Organization are actively working to mitigate polypharmacy through medication reconciliation. The purpose of medication reconciliation is to identify and resolve discrepancies that could impact patient outcomes. This is achieved by comparing the medications a patient is currently taking (or should be taking) with newly prescribed medications. The comparison considers duplications, omissions, interactions, and the necessity of continuing current medications.
The Joint Commission (2023) and the World Health Organization are actively working to mitigate polypharmacy through medication reconciliation. The purpose of medication reconciliation is to identify and resolve discrepancies that could impact patient outcomes. This is achieved by comparing the medications a patient is currently taking (or should be taking) with newly prescribed medications. The comparison considers duplications, omissions, interactions, and the necessity of continuing current medications.
Information used by physicians and other licensed professionals for medication reconciliation includes, but is not limited to, the name, dose, frequency, route, and dosage of the medication.
The risk of medication errors increases during transitions in patient care, so the reconciliation process is implemented when:
- The patient is transferred to another service or area of the organization where continuity of medication is provided.
- There is a change in the treating physician.
- The patient is discharged.
When the medication reconciliation process reveals discrepancies, these are communicated to the physician who, based on the information, will decide whether to continue, change, or discontinue the prescription.
The review of the appropriateness of the prescription serves as a safety barrier, aiming to ensure that the medication is suitable for each specific patient, considering their clinical and physiological characteristics, drug interactions, and history of allergies.
The process for reviewing the appropriateness of a prescription involves, on a patient-by-patient basis, the assessment and analysis of:
- The dose, frequency and route of administration.
- Therapeutic duplication.
- Allergies or sensitivities.
- Actual or potential interactions between the drug and other drugs or foods food.
- Variation with respect to the criteria for the use of the drug in the facility.
- The patient's weight and other physiological information.
- Other contraindications.
2.3 Incident Reporting Learning
 The World Health Organization (2022) defines an adverse drug reaction as “any unintended or unwanted noxious response that occurs at doses normally used in humans for prophylaxis, diagnosis, treatment of disease, or modification of physiological function”. While adverse drug reactions are expected, negative outcomes inherent to the pharmacological action of the drug are not always preventable, whereas medication errors are preventable. An adverse drug event is caused when the administration is omitted, or the dosage is incorrect. Such an event leads to increased morbidity or mortality in a patient.
The World Health Organization (2022) defines an adverse drug reaction as “any unintended or unwanted noxious response that occurs at doses normally used in humans for prophylaxis, diagnosis, treatment of disease, or modification of physiological function”. While adverse drug reactions are expected, negative outcomes inherent to the pharmacological action of the drug are not always preventable, whereas medication errors are preventable. An adverse drug event is caused when the administration is omitted, or the dosage is incorrect. Such an event leads to increased morbidity or mortality in a patient.
The Joint Commission (2023) defines a sentinel event as “an unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof. Serious injury specifically includes the loss of a limb or function. The phrase 'or the risk thereof' includes any process variation whose recurrence would lead to a significant likelihood of a serious adverse outcome". Sentinel events can include medication errors, adverse drug events, and medication misadventures. Sentinel events are possibly preventable.
Within the culture of Quality and Safety, the health institution and the professional staff must act proactively, meaning they should be in a permanent state of alert to identify in advance the risk situations for the patient and others. Through the practice of Risk Management, it is possible to anticipate and avoid the occurrence of adverse events in terms of processes involving medication.
When an unavoidable risk situation occurs, the reactive response of health personnel aims to mitigate the consequences of what happened. Analyzing the circumstances surrounding the event and possible causes generates a learning process to act, correct these causes, and avoid a repetition of the adverse event. When there is a commitment to the quality and safety of healthcare, the documentation of near misses or adverse events is promoted. Without any reference, it would not be possible to generate the necessary strategies to act in the prevention of the occurrence of events.
 The patient's health condition necessitates the administration of medications aimed at resolving health problems or modifying physiological conditions. However, neglecting various factors in the prescription, preparation, or administration of medications can lead to the occurrence of medication errors, near misses, adverse drug events, or sentinel events. Hence, the importance of paying close attention to these processes.
The patient's health condition necessitates the administration of medications aimed at resolving health problems or modifying physiological conditions. However, neglecting various factors in the prescription, preparation, or administration of medications can lead to the occurrence of medication errors, near misses, adverse drug events, or sentinel events. Hence, the importance of paying close attention to these processes.
Medication errors can be prevented by initiating a thorough assessment of the patient before prescribing and administering medication. Subsequently, monitoring the effects of these medications on the patient helps evaluate whether adjustments in dosage are necessary or if there are interaction effects with other drugs or food.
In the prevention of such events, it is crucial to renew the commitment to quality and safe care with a proactive attitude. Promoting the reporting and documentation of near misses and adverse drug events is vital, as this is the only way to raise awareness that potential issues may not be resolved before they occur, potentially leading to catastrophic consequences for the patient and healthcare personnel. It is in the best interest of any nursing professional to prevent medication errors and contribute to reporting and strategies aimed at preventing them.
- Hughes, R. G. (2008). Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality. https://www.ncbi.nlm.nih.gov/books/NBK2651/
- Le, J. (2022). Administration and Kinetics of Drugs. MSD Manual Costumer Version. https://www.msdmanuals.com/home/drugs/administration-and-kinetics-of-drugs/introduction-to-administration-and-kinetics-of-drugs
- Lilley, L., Collins, R., & Syndey, J. (2019). Pharmacology and the Nursing Process (9th ed.). Elsevier.
- Pan American Health Association. (2022, September 16). PAHO Urges Improved Safety in Taking and Prescribing Medicines to Reduce Harm to Patients. https://www.paho.org/es/noticias/16-9-2022-ops-insta-mejorar-seguridad-toma-prescripcion-medicamentos-para-reducir-danos/
- Pinargote-Chancay, R. R., Villegas-Chiriboga, M. E., Castillo-Merino, Y. A., Merino-Conforme, M. C., Alonso- Muñiz, G. R., Jaime-Hernandez, N. K., Riofrio-Pinagorte, C. A., Quijije-Segovia, S. K., Alcazar-Pichucho, T, M., & Pincay-Pin, V. E. (2018). Fundamentos Teóricos y Prácticos de Enfermería. Mawil Publicaciones Impresas y Digitales. https://mawil.us/wp-content/uploads/2021/04/fundamentos-teoricos-y-practicos-de-enfermeria.pdf
- Tariaq, R. A., Vashisht, R., Sinha, A., & Scherback, Y. (2023, May 2). Errors and Prevention in the Dispensing of Medicines. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK519065/
- The Joint Commission. (2023, October 4). Nursing Facility: National Patient Safety Goals for 2024. https://www.jointcommission.org/standards/national-patient-safety-goals/nursing-care-center-national-patient-safety-goals/
- World Health Organization. (2022, July 12). Medication Safety Webinar Series: Medication Safety in Polypharmacy.
https://www.who.int/news-room/events/detail/2022/07/12/default-calendar/medication-safety-webinar-series-medication-safety-in-polypharmacy
The following links do not belong to Tecmilenio University, when accessing to them, you must accept their terms and conditions.
Readings
- Canadian Patient Safety Institute. (2020). The Safety Competencies: Enhancing Patient Safety Across (2nd ed.). https://www.patientsafetyinstitute.ca/en/toolsResources/safetyCompetencies/Documents/CPSI-SafetyCompetencies_EN_Digital.pdf%23search=Competencies
Video
- Medical Dialogues. (2022, April 30). Journal Club- Polypharmacy A Global Risk Factor for Elderly People [Video]. YouTube. https://www.youtube.com/watch?v=N39OS_kv-7w
La obra presentada es propiedad de ENSEÑANZA E INVESTIGACIÓN SUPERIOR A.C. (UNIVERSIDAD TECMILENIO), protegida por la Ley Federal de Derecho de Autor; la alteración o deformación de una obra, así como su reproducción, exhibición o ejecución pública sin el consentimiento de su autor y titular de los derechos correspondientes es constitutivo de un delito tipificado en la Ley Federal de Derechos de Autor, así como en las Leyes Internacionales de Derecho de Autor.
El uso de imágenes, fragmentos de videos, fragmentos de eventos culturales, programas y demás material que sea objeto de protección de los derechos de autor, es exclusivamente para fines educativos e informativos, y cualquier uso distinto como el lucro, reproducción, edición o modificación, será perseguido y sancionado por UNIVERSIDAD TECMILENIO.
Queda prohibido copiar, reproducir, distribuir, publicar, transmitir, difundir, o en cualquier modo explotar cualquier parte de esta obra sin la autorización previa por escrito de UNIVERSIDAD TECMILENIO. Sin embargo, usted podrá bajar material a su computadora personal para uso exclusivamente personal o educacional y no comercial limitado a una copia por página. No se podrá remover o alterar de la copia ninguna leyenda de Derechos de Autor o la que manifieste la autoría del material.