Safety and Infection Control / 08
Make sure to:
- Maintain surgical asepsis.
- Promote standard precautions.
- Adhere to transmission-based precautions.
 Nurses have a responsibility to maintain a safe environment in their healthcare facility for clients, their families, members of the healthcare team, and patrons. One way to achieve this is by preventing infection, which can be harmful to those who become infected and costly for healthcare facilities. Infectious agents include bacteria, viruses, fungi, parasites, and prions (Burke, 2023). These infectious agents may reside in humans, water, animal, or the soil, and their direct or indirect transmission to a susceptible person (a host) can result in an infection (Burke, 2023).
Nurses have a responsibility to maintain a safe environment in their healthcare facility for clients, their families, members of the healthcare team, and patrons. One way to achieve this is by preventing infection, which can be harmful to those who become infected and costly for healthcare facilities. Infectious agents include bacteria, viruses, fungi, parasites, and prions (Burke, 2023). These infectious agents may reside in humans, water, animal, or the soil, and their direct or indirect transmission to a susceptible person (a host) can result in an infection (Burke, 2023).
Clients who are immunosuppressed, those who have undergone surgery or surgeries, and individuals undergoing treatments such as chemotherapy, indwelling urinary catheter placement, and endotracheal tube insertion are at risk for acquiring infections (Burke, 2023). Pseudomonas aeruginosa, Candida albicans, Enterococcus, E. coli, and Staphylococcus are the primary infectious agents in a healthcare setting (Burke, 2023). Infections acquired in a healthcare facility usually occur during admission and are transmitted by the hands of the healthcare providers (Burke, 2023).
In this learning experience, the learner will be taught how to prevent infection through surgical asepsis, standard precautions, and transmission-based precautions.
1.1 Surgical Asepsis
 Surgical asepsis, also referred to as the surgical technique, is one of the ways to prevent the spread of infection by eliminating all microorganisms (Burke, 2023). This is applicable to clients who do not have intact skin and those whose internal organs are being accessed and/or treated. For example, during wound care, surgeries, and invasive procedures, such as the insertion of urinary catheter, central venous lines, peripheral intravenous lines, and when administering intravenous medication (Burke, 2023).
Surgical asepsis, also referred to as the surgical technique, is one of the ways to prevent the spread of infection by eliminating all microorganisms (Burke, 2023). This is applicable to clients who do not have intact skin and those whose internal organs are being accessed and/or treated. For example, during wound care, surgeries, and invasive procedures, such as the insertion of urinary catheter, central venous lines, peripheral intravenous lines, and when administering intravenous medication (Burke, 2023).
Personal protective equipment, such as head covering, mask, sterile gloves, gowns and sometimes googles, is required during surgeries or procedures.
According to Burke (2023), it is important to set up and maintain asepsis by:
- Wearing a sterile gown and gloves if a member of the sterile team.
- Wearing a sterile mask if indicated.
- Designating and creating a sterile area or field.
- Creating and maintaining a one-inch non-sterile area around the edge of the sterile field.
- Placing only sterile items in the sterile field.
- Do not:
- Turn your back to the sterile field.
- Lean over the sterile field.
- Cough or sneeze on the sterile field, as this will contaminate the area.
- Keeping the sterile field above the waist, dry, and pouring sterile liquids with the labels facing upwards.
- Discarding and redoing the entire sterile field if there was failure to adhere to the above at any point during the surgery, procedure, or treatment.
It is important to dispose of the PPE according to the facility policy and procedure.
Standard Precautions
 Standard precautions, also known as universal precautions, are techniques used to prevent the spread of infection resulting from contaminated body fluids; they apply to all clients, regardless of their infection status (Burke, 2023). This is facilitated by handwashing, the use of gloves, gown, mask, eye protection, or personal protective equipment (PPE), as well as environment control and careful consideration of client placement (Kaplan Nursing, 2023).
Standard precautions, also known as universal precautions, are techniques used to prevent the spread of infection resulting from contaminated body fluids; they apply to all clients, regardless of their infection status (Burke, 2023). This is facilitated by handwashing, the use of gloves, gown, mask, eye protection, or personal protective equipment (PPE), as well as environment control and careful consideration of client placement (Kaplan Nursing, 2023).
- Handwashing: It is important to wash hands before and after each client contact and when donning or removing gloves, in addition to after being exposed to body fluids or blood (Kaplan Nursing, 2023). Infections acquired in healthcare facilities typically occur during admission and are transmitted by the hands of healthcare providers; therefore, nurses and other healthcare team members must wash their hands properly (Burke, 2023).
- Gloves: Donn clean, non-sterile gloves before touching a client’s mucous membrane, non-intact skin, articles contaminated with blood, and body fluids such as secretions and excretions (Kaplan Nursing, 2023). It is also important to change gloves before and after each task/procedure, before and after coming in contact with each client, and to remove gloves immediately after use and before touching items and surfaces in the client’s spaces (Kaplan Nursing, 2023).
- Personal Protective Equipment (PPE): This equipment protects nurses from direct contact with clients’ blood and/or body fluids, which may or may not be infected. Nurses should wear a face shield, eye protection, or mask during activities that could result in blood and/or body fluids coming in contact with the eyes, nose, and/or mouth (Kaplan Nursing, 2023). Additionally, nurses must wear clean non-sterile gowns if they are going to engage in activities that could cause blood and/or body fluids to get on their skin or soil their clothes (Kaplan Nursing, 2023).
- Environment Control: Nurses can prevent infection by using a mouthpiece or a resuscitation bag instead of direct mouth-to-mouth resuscitation and by being mindful of the safe handling of used sharps/needles (Kaplan Nursing, 2023). It is important to discard needles and sharps in accordance with the policy and procedure of the facility. For example, do not recap needles before discarding them, and discard needles and sharps in designated puncture-resistant containers (Kaplan Nursing, 2023).
- Client Placement: Clients are placed in either a private or shared room. Clients who are not attentive to their hygiene, infants, children, and clients with altered mental status, who are on infection control precautions should be placed in a private room (Kaplan Nursing, 2023). On the other hand, room sharing or “cohorting” can occur based upon how the infectious agent is transmitted and the epidemiology of the diseases (Kaplan Nursing, 2023).
Adhering to facility policy and procedure regarding the transport of infectious clients is crucial. If required, clients may need to wear a mask during transport, healthcare team members should be informed of arrival and precautions prior to transfer, and clients should be educated about transmission prevention (Kaplan Nursing, 2023).
1.3 Transmission-based Precaution
 Transmission-based precautions refer to preventing the spread of infection from clients with suspected or known highly transmissible infection, using airborne, droplet, and/or contact precautions (Kaplan Nursing, 2023).
Transmission-based precautions refer to preventing the spread of infection from clients with suspected or known highly transmissible infection, using airborne, droplet, and/or contact precautions (Kaplan Nursing, 2023).
Airborne precautions are employed for infectious microorganisms that are less than 5 microns in size and are transmitted through the air in the form of dust particles or airborne droplets (Kaplan Nursing, 2023). This applies to clients with M. tuberculosis, measles (rubeola), varicella (chicken pox), disseminated zoster (shingles) (Kaplan Nursing, 2023).
Droplet precautions are utilized for infectious microorganisms that are larger than 5 microns in size and are transmitted by “infectious droplets” (Kaplan Nursing, 2023). Transmission may occur through the mucous membrane of the mouth or nose during a cough, sneeze, speaking, or certain medical procedure such as bronchoscopy or suctioning (Kaplan Nursing, 2023). Clients with Diphtheria, Group A Streptococcus pneumonia, pneumonia or meningitis secondary to N. meningitidis or H. influenza Type B, Rubella, mumps, and pertussis should be placed on droplet precaution (Kaplan Nursing, 2023).
Contact precautions should be followed when nurses engage in activities that require physical contact with clients, such as during turning and bathing, or when touching inanimate objects that are contaminated (Kaplan Nursing, 2023). Clients with the following conditions should be placed on contact precautions: herpes zoster/simplex, scabies, rotavirus, hepatitis, respiratory syncytial virus (RSV), pediculosis, multidrug-resistant organisms such as MRSA and Vancomycin-resistant organisms, and Clostridioides difficile (Kaplan Nursing, 2023). It is important to remove the PPE before exiting the client’s room and wash hands with an antimicrobial agent. Table 1 summarizes the actions that nurses should take during each of the three types of precautions.
Table 1
Summary of Actions/Interventions to take During Airborne, Droplet, and Contact Precautions
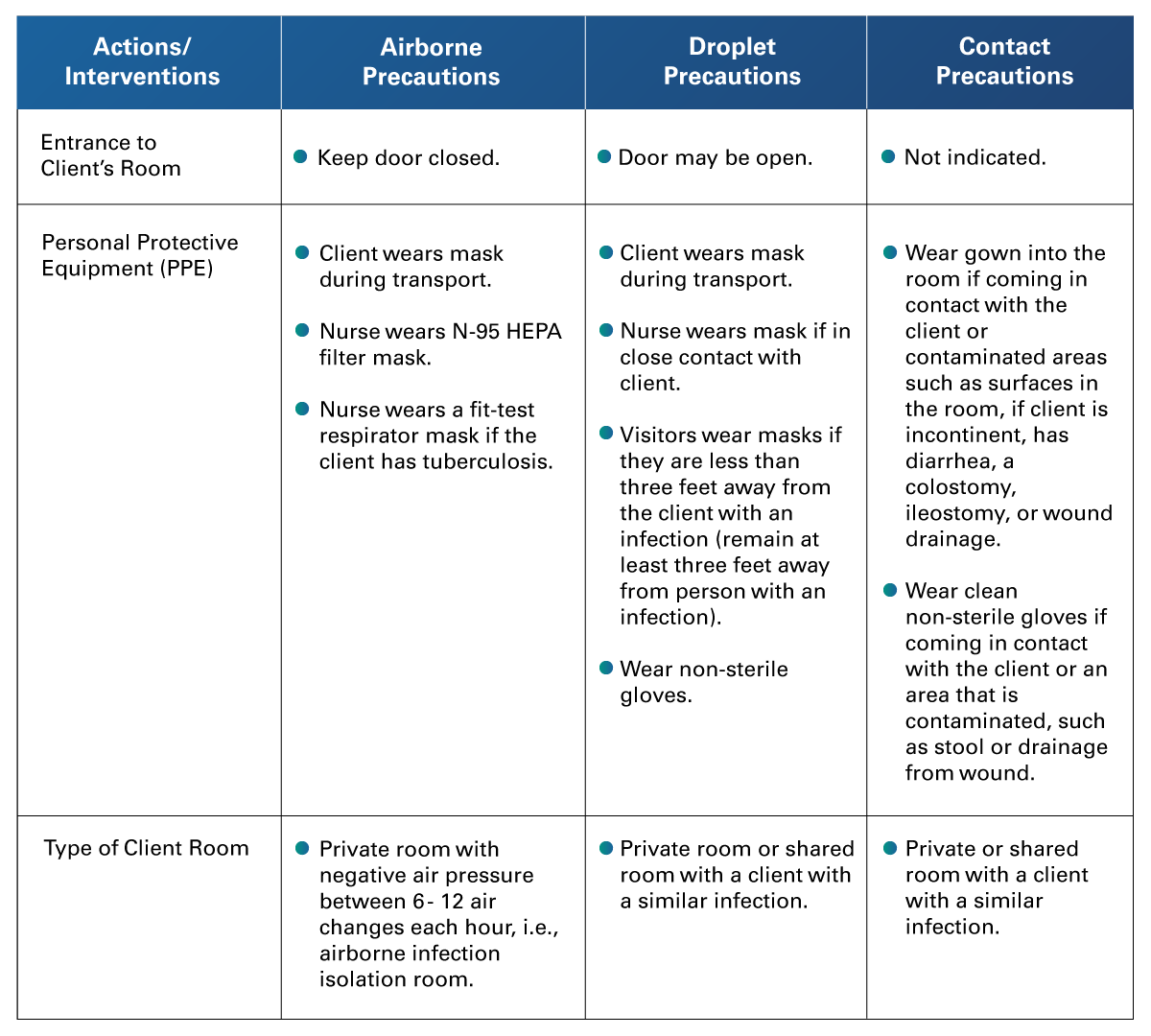 Adapted from Kaplan Nursing. (2023). NCLEX-RN Content Review Guide. Kaplan Test Prep.
Adapted from Kaplan Nursing. (2023). NCLEX-RN Content Review Guide. Kaplan Test Prep.
 Upon concluding this learning experience, learners will acquire a deeper understanding of preventing infection in the clinical setting, with emphasis on surgical asepsis, standard precautions, and transmission-based precaution.
Upon concluding this learning experience, learners will acquire a deeper understanding of preventing infection in the clinical setting, with emphasis on surgical asepsis, standard precautions, and transmission-based precaution.
The resources will enable learners to further expand their knowledge and gain proficiency in preventing infection in their healthcare facilities. The ultimate goals include achieving success in both the NCLEX examination and in the workplace.
After reviewing the resources, identify areas in which improvements can be made and concentrate on those specific areas.
- Burke, A. (2023, August 24). Standard Precautions, Transmission-based, Surgical Asepsis: NCLEX-RN. https://www.registerednursing.org/nclex/standard-precautions-transmission-based-surgical-asepsis/
- Kaplan Nursing. (2023). NCLEX-RN Content Review Guide (9th ed.). Kaplan Test Prep.
The following links do not belong to Tecmilenio University, when accessing to them, you must accept their terms and conditions.
Readings
- Habboush, Y., Yarrarapu, S. N. S., & Guzman, N. (2023). Infection Control. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK519017/
Videos
- Lecturio Nursing. (2021, July 15) What Causes an Infection?: Breaking the Chain of Infection | Lecturio Nursing Fundamentals/Theory [Video]. YouTube. https://youtu.be/EXtTTG6YYAI
La obra presentada es propiedad de ENSEÑANZA E INVESTIGACIÓN SUPERIOR A.C. (UNIVERSIDAD TECMILENIO), protegida por la Ley Federal de Derecho de Autor; la alteración o deformación de una obra, así como su reproducción, exhibición o ejecución pública sin el consentimiento de su autor y titular de los derechos correspondientes es constitutivo de un delito tipificado en la Ley Federal de Derechos de Autor, así como en las Leyes Internacionales de Derecho de Autor.
El uso de imágenes, fragmentos de videos, fragmentos de eventos culturales, programas y demás material que sea objeto de protección de los derechos de autor, es exclusivamente para fines educativos e informativos, y cualquier uso distinto como el lucro, reproducción, edición o modificación, será perseguido y sancionado por UNIVERSIDAD TECMILENIO.
Queda prohibido copiar, reproducir, distribuir, publicar, transmitir, difundir, o en cualquier modo explotar cualquier parte de esta obra sin la autorización previa por escrito de UNIVERSIDAD TECMILENIO. Sin embargo, usted podrá bajar material a su computadora personal para uso exclusivamente personal o educacional y no comercial limitado a una copia por página. No se podrá remover o alterar de la copia ninguna leyenda de Derechos de Autor o la que manifieste la autoría del material.