Physiological Adaptation / 06
Make sure to:
- Recall necessary knowledge to determine the clients’ needs with hemodynamics pathologies.
- Determine techniques and methods to assess clients’ symptoms and parameters.
- Quote nursing-based evidence interventions to assist the client with hemodynamics pathologies.
 Physiological adaptation is defined by Estaphan et al. (2023) as an organism's ability to adapt and adjust to acute and chronic changes in both internal and external environments throughout its lifespan.
Physiological adaptation is defined by Estaphan et al. (2023) as an organism's ability to adapt and adjust to acute and chronic changes in both internal and external environments throughout its lifespan.
This ability, in tandem with the advances in medicine, has extended the life expectancy of the average person. Paradoxically, acute myocardial infarctions (AMIs) and other cardiovascular diseases represent the most common causes of mortality and are even appearing at younger ages.
In this learning experience, the matters of physiological adaptations related to hemodynamics will be addressed. The field of hemodynamics covers the flow of blood throughout the organism and the physical structures (like veins, lungs and heart) through which it mobilizes.
2.1 Performing Interventions to Improve Client Cardiovascular Status
 In current times, the daily habits and lifestyle of most people have presented a switch from active and in the countryside to sedentary and urban. Along with this trend, industrialized foods have become cheaper and more readily available, resulting in convenience. The downside to them is that they are high in harmful substances, such as sweeteners, colorings, sodium, fat and simple carbohydrates.
In current times, the daily habits and lifestyle of most people have presented a switch from active and in the countryside to sedentary and urban. Along with this trend, industrialized foods have become cheaper and more readily available, resulting in convenience. The downside to them is that they are high in harmful substances, such as sweeteners, colorings, sodium, fat and simple carbohydrates.
The American Heart Association (AHA) has made the prevention of cardiovascular diseases (CVD) a priority strategy. It has issued a guideline that is important for health personnel to understand, adhere to, and act upon in favor of patients.
The AHA (2020) carried out a rigorous systematic review, from which the following recommendations originated:
- Promote a lifelong healthy lifestyle to prevent CVD.
- Working in multidisciplinary teams.
- Taking into account the patients’ social determinants.
- It is recommended to evaluate cardiovascular risk in individuals younger than 40, promoting healthy lifestyles before starting pharmacological therapy.
- All adults should consume a healthy diet that emphasizes the intake of vegetables, fruits, nuts, whole grains, lean vegetable or animal protein, and fish. Minimizing the intake of trans fats, red meat, processed red meats, refined carbohydrates, and sweetened beverages. For adults with overweight and obesity, counseling and caloric restriction are recommended for achieving and maintaining weight loss.
- Physical activity for adults is recommended in at least 150 minutes per week of moderate or 75 minutes per week of vigorous exercise.
- For adults with type 2 diabetes, a considerable lifestyle change is recommended. Metformin is first-line therapy, followed by consideration of a sodium-glucose cotransporter 2 inhibitor or a glucagon-like peptide-1 receptor agonist.
- Healthcare providers should identify tobacco users and assist them in quitting smoking.
- Aspirin should be used infrequently in the routine primary prevention of Atherosclerotic Cardiovascular Disease (ASCVD) because of a lack of net benefit.
- Statin therapy is the first-line treatment for primary prevention of ASCVD in patients with elevated low-density lipoprotein cholesterol levels (≥190 mg/d). Those with diabetes mellitus, who are 40 to 75 years of age, and those determined to be at sufficient ASCVD risk after a clinician–patient risk discussion.
- Nonpharmacological interventions are recommended for all adults with elevated blood pressure or hypertension. For those requiring pharmacological therapy, the target blood pressure should generally be <130/80 mm Hg (American Heart Association, 2020).
It is important to remember that monitoring patients to adhere to treatment is an important success factor, in addition to having social support networks, especially family.
2.2 Identifying Cardiac Rhythm Strip Abnormalities
 The heart, located in the mediastinum of the thorax, is slightly to the left. It is shaped like an inverted triangle, extending superiorly to inferiorly and diagonally from right to left in an anteroposterior direction. Structurally, it is flanked by the lungs on either side and positioned anteriorly to the thoracic cage. The heart functions as a pump. Through its two upper chambers (or atria) and its two lower chambers (or ventricles), the heart makes the blood circulate through blood vessels. It is of note that arteries carry oxygenated blood while veins carry deoxygenated blood.
The heart, located in the mediastinum of the thorax, is slightly to the left. It is shaped like an inverted triangle, extending superiorly to inferiorly and diagonally from right to left in an anteroposterior direction. Structurally, it is flanked by the lungs on either side and positioned anteriorly to the thoracic cage. The heart functions as a pump. Through its two upper chambers (or atria) and its two lower chambers (or ventricles), the heart makes the blood circulate through blood vessels. It is of note that arteries carry oxygenated blood while veins carry deoxygenated blood.
The chambers of the heart are divided into left and right. From the right side, through the superior and inferior vena cava, deoxygenated blood arrives from the body, and passes from the right atrium to the right ventricle through the tricuspid valve. From the left ventricle, blood comes out through the pulmonary arteries to the lungs to leave carbon dioxide toxins and receive oxygen. This is called minor circulation. From the lungs come the pulmonary veins responsible for carrying oxygenated blood to the left ventricle through the bicuspid or mitral valve to be distributed throughout the body through the aorta artery and all its branches. This is called major circulation.
The heart is made of striated muscle whose contractility depends on an electrical impulse generated in the atrioventricular node, located in the right ventricle. From there, the energy travels to the bundle of His and while doing so, it depolarizes the cells of both atria, which contract and empty the contents of their chambers, sending blood to the ventricles. The energy continues its course through the left and right branches of the bundle of His and its branches, causing the contraction of the ventricles that empty their chambers, sending blood to the lungs and body, respectively. While this occurs, the relaxed chambers of the atria receive blood from the body (right side) and lungs (left side).
The heart's electrical activity is recorded by an Electrocardiogram. This device uses electrodes and conductive gel to form an imaginary triangle, known as Einthoven's triangle, to capture the heart’s electrical signals.
Thus, the electrical trace can be recorded from any of the three edges of the triangle or bipolar leads, which are called DI, DII and DIII. These edges are connected due to the electrodes LA (Left Arm), RA (Right Arm), and LL (Left Leg).
Figure 1
Electrodes Position to Form Bipolar Leads
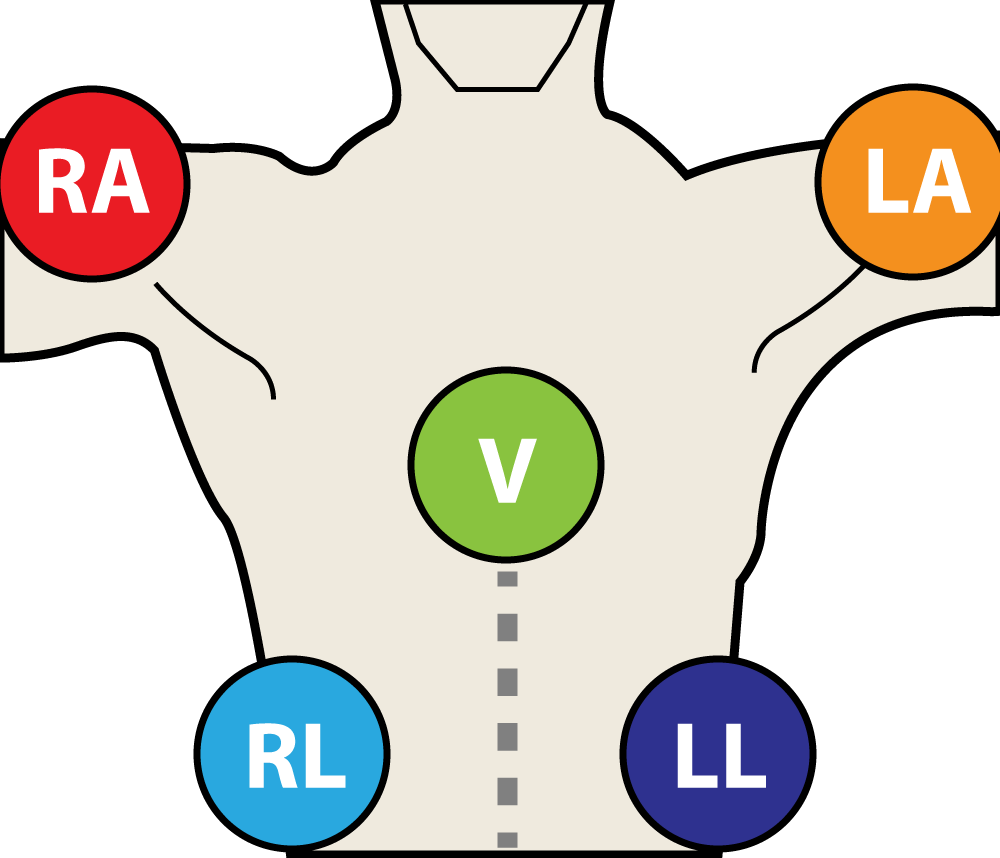 Adapted from Tung, R. T. (2021). Electrocardiographic Limb Leads Placement and Its Clinical Implication: Two Cases of Electrocardiographic Illustrations. Kansas Journal of Medicine,14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8415387/
Adapted from Tung, R. T. (2021). Electrocardiographic Limb Leads Placement and Its Clinical Implication: Two Cases of Electrocardiographic Illustrations. Kansas Journal of Medicine,14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8415387/
For greater detail, six unipolar leads, namely V1, V2, V3, V4, V5, and V6, are placed as follows:
Table 1
Positions for V1 to V6 Leads
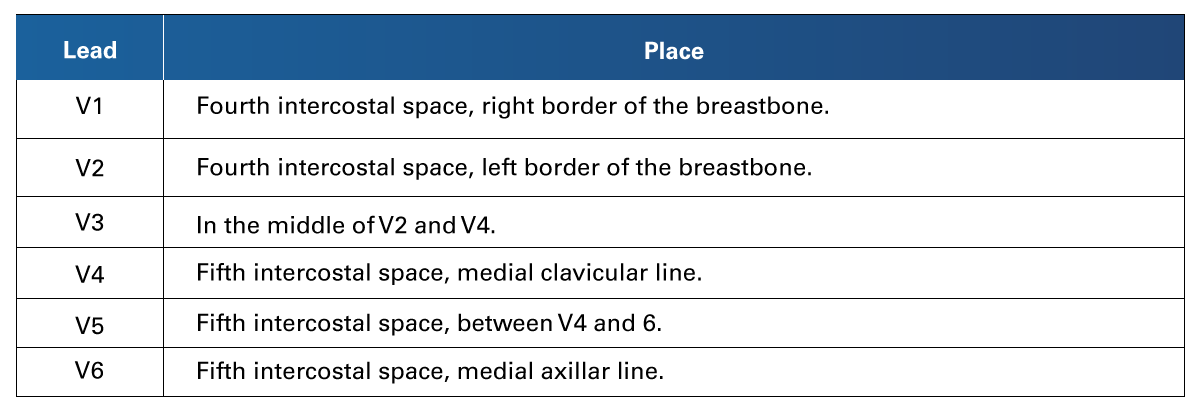 Retrieved from Tung, R. T. (2021). Electrocardiographic Limb Leads Placement and Its Clinical Implication: Two Cases of Electrocardiographic Illustrations. Kansas Journal of Medicine,14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8415387/
Retrieved from Tung, R. T. (2021). Electrocardiographic Limb Leads Placement and Its Clinical Implication: Two Cases of Electrocardiographic Illustrations. Kansas Journal of Medicine,14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8415387/
Figure 2
Position for Monopolar Leads
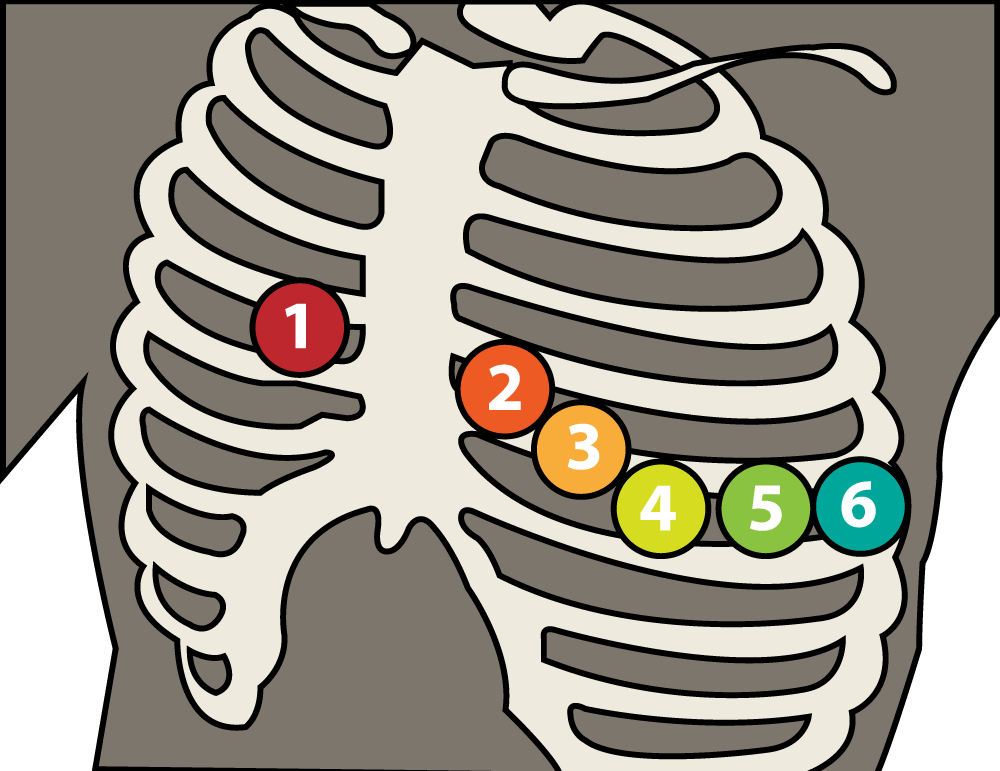 Adapted from Tung, R. T. (2021). Electrocardiographic Limb Leads Placement and Its Clinical Implication: Two Cases of Electrocardiographic Illustrations. Kansas Journal of Medicine, 14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8415387/
Adapted from Tung, R. T. (2021). Electrocardiographic Limb Leads Placement and Its Clinical Implication: Two Cases of Electrocardiographic Illustrations. Kansas Journal of Medicine, 14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8415387/
The electrocardiogram is recorded on a grid sheet. On the horizontal plane, the boxes represent time. The large squares represent 5 millimeters (mm) across, with 5 small squares representing 1 mm. 1 mm represents 0.04 seconds (sec) and 5 mm represents 0.20 sec. In the vertical plane the boxes represent volts. One millimeter is equal to 0.1 millivolt (mv).
The record is based on a flat line called isoelectric, which means an absence of electricity. All upward strokes are considered positive and downward strokes are considered negative. The curves are called waves, the isoelectric line between one wave and another is called a segment.
P-waves represent atrial contraction. The PR interval represents the time taken for excitation to spread from the sino-atrial (SA) node across the atrium and down to the ventricular muscle via the bundle of His. The QRS interval registers the ventricular contraction. The ST segment depicts ventricular relaxation. And finally, the T-wave shows the ventricular repolarization (Kusumoto, 2020).
Figure 3
Electrocardiogram Traces
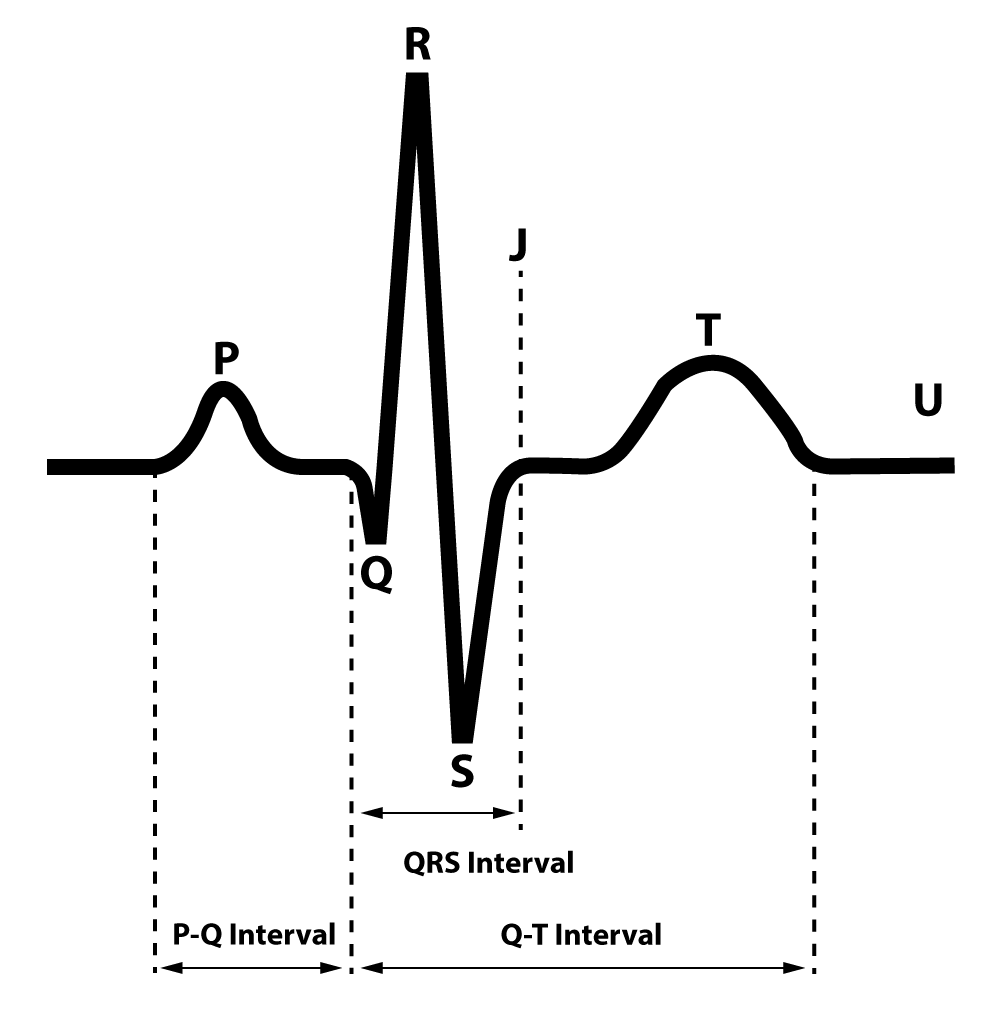 Adapted from Kusumoto, F. (2020). ECG Interpretation: From Pathophysiology to Clinical Application. Springer Nature.
Adapted from Kusumoto, F. (2020). ECG Interpretation: From Pathophysiology to Clinical Application. Springer Nature.
The normal duration of ECG segments is standardized. The PR interval commonly lasts 0.12 – 0.2 secs (which is the same as 3-5 small squares). The QRS should be less than 0.12 secs (or 3 small squares). Lastly, the QTc interval should last between 0.38 and 0.42 secs, in a healthy heart.
The interpretation of an ECG has many levels of interpretation. General medical practitioners and nursing professionals should be able to understand at the basic level, to take the most information out of it before complementing it with the attention provided by the cardiologist.
The first thing needed to do is confirm the patient's details. Gather all the information necessary to identify the person's history and current condition and be able to develop possible hypotheses about what is happening.
Then, one must determine the heart rate. Cardiac frequency can be calculated by counting the QRS in ten seconds of lead II and multiplying x 6 or counting the large squares from one R wave to another and dividing by 300.
Please remember that the normal rate is between 60 and 100 beats per minute (bpm), a frequency that is less than 60 is bradycardia and over is 100 tachycardia.
After determining the rate, the next aspect to analyze is rhythm. Regular rhythms have a constant distance between R waves.
There is a global direction term for the conduction of the heart known as the Axis. The axis is the sum of all the electrical activity in the heart; if the net deflections in leads I and aVF are positive, then the axis is normal.
Going over the different lines and segments, the P wave represents the contraction of the atria, a flat P represents less electrical energy, and a high P means that the heart made a great effort to push blood to the rest of the body. Normally, this happens in cardiac hypertrophy or increased cardiac output. Left atrial hypertrophy could be represented by bifid P-waves or mitral waves. Pericarditis can cause depression of P-wave. Please keep in mind that an ECG without P wave indicates the absence of working atria.
The PR interval is a space in which it takes time for the electrical impulse from the atria to reach the ventricles. When there is tachycardia, this interval is shortened and may disappear in high tachycardia. On the contrary, the lengthening of this segment may represent a blockage of the electrical impulse from the atria to the ventricles.
If the Q-wave is bigger than 0.04 y 0.02 from deep it indicates more effort of contraction of the heart muscles.
QRS complexes bigger than 0.12 secs indicate more effort of contraction of the heart muscles due to hypertrophy that also causes tall QRS, hyperkalemia, paced rhythm, or use of tricyclic antidepressants, among other causes.
Elevation of the ST segment is indicative of infarction, and depression of the ST segment is indicative of digoxin toxicity. The ST depression will be down sloping (“reverse tick” sign).
The QT interval is from the start of the q-wave and the end of the t-wave. This segment is especially sensitive to electrolyte imbalances.
The T wave is the depolarization of the ventricles and can be affected by electrolyte imbalances, ischemia, or digoxin.
Lastly, it is crucial to remember two points: ventricular tachycardia and ventricular fibrillation are the rhythms susceptible to defibrillation, and the isoelectric line represents total cardiac arrest.
2.3 Managing the Care of a Client Receiving Hemodialysis or Continuous Renal Replacement Therapy
 Kidney disease is an acute, chronic, or of undetermined time condition that affects a significant portion of the population. The main causes are poor water intake, type 2 diabetes, hypertension, retention of urine for prolonged periods, and the intake of harmful beverages such as alcohol or soft drinks, leading to vascular, glomerular, interstitial tubule diseases, or obstructive uropathies. Because of this, the kidney progressively or acutely decreases its Glomerular Filtration Rate (GFR) and stops filtering toxins, which remain free in the blood and damage cellular tissue. Consequently, as the excess volume produced is not being properly eliminated, this condition leads to hypervolemia. By definition, stage 5 of renal disease requires renal replacement. The renal replacement techniques available to date are dialysis, hemodialysis, and kidney transplant.
Kidney disease is an acute, chronic, or of undetermined time condition that affects a significant portion of the population. The main causes are poor water intake, type 2 diabetes, hypertension, retention of urine for prolonged periods, and the intake of harmful beverages such as alcohol or soft drinks, leading to vascular, glomerular, interstitial tubule diseases, or obstructive uropathies. Because of this, the kidney progressively or acutely decreases its Glomerular Filtration Rate (GFR) and stops filtering toxins, which remain free in the blood and damage cellular tissue. Consequently, as the excess volume produced is not being properly eliminated, this condition leads to hypervolemia. By definition, stage 5 of renal disease requires renal replacement. The renal replacement techniques available to date are dialysis, hemodialysis, and kidney transplant.
In Mexico, dialysis is the most common procedure for treating renal disease. It is a procedure in which fluid enters the abdomen to carry out the process of diffusion of the patient's toxins into the dialysis fluid through the peritoneum membrane. There are two types of dialysis: Manual or Continuous Ambulatory Peritoneal Dialysis (CAPD) and automated or Automatic Peritoneal Dialysis (APD).
In CAPD, the warm bag of dialysate fluid is connected to the catheter in the patient’s abdomen by the nurse or relatives, procuring a sterile technique. After this, the liquid must be allowed to be introduced by gravity, letting the liquid rest according to the medical indications. Finally, the liquid will be released into the twin dialysate bag.
For APD, the twin bag is connected to a machine which is programmed to make the necessary fluid exchanges as dictated by the medical orders.
Now, for hemodialysis, the patient is connected to a machine through which the body's blood passes and is cleaned through the machine's filters. This technique is ideal due to its effectiveness in purifying the blood, but it is not the first treatment of choice in developing countries, due to the technology and resources needed.
Ideally, renal substitution therapy would involve a kidney transplant. However, waiting lists are long, and the patient cannot always wait. For the procedure to be performed, the recipient and the donor must be compatible. The patient undergoes a delicate surgical process. In addition to the burden of post-surgical recovery, they must also deal with psychological recovery and adapt to their new living conditions.
When caring for a patient receiving renal substitution therapy, the general nursing objectives are to keep an adequate record of the patient's fluid balance, which includes monitoring vital signs such as respiratory rate, heart rate, and arterial pressure and being aware of symptoms of hypervolemia or hypovolemia. For hypovolemia, orthostatic vital signs are an important clue (Goyal et al., 2023).
In this condition, nutrition should restrict fluids and salt according to medical treatment and avoid meats and phosphorus, which are present in foods like beans. Protein intake is usually increased because albumin is cleared during therapies. It is important to try to maintain an adequate nutritional status, distinguishing the weight of lean mass from the weight of water. The patient should be educated about foods that help reduce nausea, such as crackers and supplements that provide vitamins and proteins, as indicated by the treatment. Bananas and tomatoes will be recommended to replace potassium loss due to their clearance during therapy.
Physical activity is often compromised, so it is important to suggest a low-impact exercise routine to preserve muscle mass. Muscle stretching exercises and massage should be included since cramps are present due to the loss of electrolytes during therapy.
Considering the impact that social networks have in current times, managing social and government support networks to the extent possible would be a recommended practice, since this is a chronic and costly disease. Support groups, non-governmental organizations and social connection to others facing these problems, would provide a support system to navigate difficult circumstances.
Individuals with kidney failure often experience sleep disturbances, which can be caused by the volume of fluids in the abdomen, or the discomfort generated by the accumulation of toxins. It is important to teach a sleep hygiene routine, increase daytime naps and evaluate the use of melatonin as an inducer of night rest.
The alteration of blood circulation secondary to the increase in portal pressure and fluid stagnation causes people with kidney failure to have difficulty maintaining body temperature. Additionally, during dialysis therapy, there is a risk of heat loss through convection. The nurse must ensure the provision of physical means to maintain an adequate temperature, such as securing warm blankets nearby and knowing the process to adjust the air conditioning of the area (or knowing who to contact for it) in case it is needed.
Finally, regarding the cares related to hygiene, the skin tends to dry out due to the accumulation of urea and toxins, making it more prone to injuries. Adequate moisturization must be provided, and special care must be taken at the entry ports for therapies, whether by catheter or fistula, to avoid infection.
2.4 Managing the Care of a Client with Alteration in Hemodynamics
 The risk with hemodynamic alterations is that tissues might suffer hypoperfusion due to poor circulation. The organs to pay special attention to are the heart, kidneys, and lungs. Proper care and management of the patient in these conditions prevents the development of serious damage and provides a shorter time for rehabilitation. The most common consequence of hemodynamic alterations is heart failure, which can be analyzed individually as left-sided failure or right-sided failure.
The risk with hemodynamic alterations is that tissues might suffer hypoperfusion due to poor circulation. The organs to pay special attention to are the heart, kidneys, and lungs. Proper care and management of the patient in these conditions prevents the development of serious damage and provides a shorter time for rehabilitation. The most common consequence of hemodynamic alterations is heart failure, which can be analyzed individually as left-sided failure or right-sided failure.
In left-sided failure, the patient may present dyspnea, orthopnea, pleural effusion, Cheyne-Stokes respirations, crackles by pulmonary edema, blood sputum, decreased renal function, edema, cerebral anoxia, fatigue, muscle weakness, and S3 gallop, according to Kaplan Nursing (2023).
For right-sided failure, it is common to observe edema, abdominal pain, nausea, and coolness of the extremities, which is secondary to venous congestion in the major organs (Kaplan Nursing, 2023). In case the heart failure progresses, the patient may experience cardiogenic shock, which is a type of acute heart failure that requires emergency intervention. During cardiogenic shock, the heart fails as a pump, generating lower output and altering tissue perfusion. If uncontrolled, this may lead to multiple organ failure.
When assessing a patient for these alterations, the first aspect to inspect is the patient’s general appearance, then their state of consciousness, and finally the monitoring of their vital signs. The signs of alarm to look out for are diaphoresis, tachycardia, tachypnea, a systolic blood pressure lower than 90 mmHg, urine output less than 30 mL/hr, loss of corporal temperature or disorientation.
The diagnoses expected of the nursing professional to be able to detect are decreased cardiac output, intolerance towards activity, anxiety, deficient knowledge, impaired gas exchange, and ineffective tissue perfusion (especially cerebral).
The interventions to be carried out by the nursing professional for patients of this type are the following:
- Monitoring the patient’s vital signs, cardiac trace (including presence of pain), and urinary output with a urinary catheter.
- Provide oxygen, if necessary, and prepare in case of intubation or insertion of an intro-aortic balloon pump.
- Installing IV lines, starting fluid balances account, and monitoring in case of electrolyte imbalances.
- Maintaining corporal temperature.
- Pharmacological treatment could consist of IV morphine sulfate, diuretics, nitrates, vasopressors, and positive inotropes.
- If indicated, prepare for immediate reperfusion procedures such as percutaneous transluminal coronary angioplasty (PTCA) or coronary artery bypass graft, or insertion of pulmonary artery Swan-Ganz catheter to assess the degree of failure (Silvestri et al., 2021).
- Security is crucial; so, bed protection should be provided for the patient in case of mental confusion.
- Provide CPR as American Heart Association recommends if it is necessary (American Heart Association, 2020).
- Preparing the patient to procedure and monitoring hemodynamics with central venous pressure (CVP), pulmonary artery pressures, and mean arterial pressure (MAP) (Silvestri et al., 2021).
Regarding central venous pressure (CVP), this is the pressure of the superior vena cava, measured with a central catheter. Normal rates are usually around 3 to 8 mmHg. For interpretation, lower levels are indicative of hypovolemia, while greater values indicate hypervolemia. To measure CVP, the nurse needs to place the patient in a supine position and align the CVP line directly with the mid-axillary line. Allow the solution to flow into the catheter rule and observe as the solution descends, registering the number on the rule where the solution pauses the longest.
As a final consideration, the Mean Arterial Pressure (MAP) is the average systemic pressure. Expected values are from 70 to 105, and it can be calculated through the formula 2(DP) + SP)/3, where “DP” is diastolic pressure and “SP” is systolic pressure.
 As presented, adequate body homeostasis is achieved when proper oxygenation and tissue nutrition is sustained. Every person is at risk of developing pathological conditions, so it becomes imperative to detect early signs and address them with the right treatment promptly. The disease can be fully avoided if detection and treatment are done in time. The two major organs in the process of hemodynamics are the heart and the kidney, so keeping an eye on the vital signs and test results that speak of their function are good practices for any nursing professional interested in providing high-quality care.
As presented, adequate body homeostasis is achieved when proper oxygenation and tissue nutrition is sustained. Every person is at risk of developing pathological conditions, so it becomes imperative to detect early signs and address them with the right treatment promptly. The disease can be fully avoided if detection and treatment are done in time. The two major organs in the process of hemodynamics are the heart and the kidney, so keeping an eye on the vital signs and test results that speak of their function are good practices for any nursing professional interested in providing high-quality care.
- American Heart Association. (2020). Adult Cardiac Arrest Algorithm. https://cpr.heart.org/-/media/CPR-Files/CPR-Guidelines-Files/Algorithms/AlgorithmACLS_CA_200402.pdf
- Estaphan, S., Wadley, G. D., Todd, G., Towstoless, M., Hryciw, D. H., Lexis, L., Hayes, A., Tangalakis, K., & Force, T. (2023). Unpacking and Validating the Physiological Adaptation Core Concept of Physiology. Advances in Physiology Education, 47(4), 831-837. https://doi.org/10.1152/advan.00083.2023
- Goyal, A., Daneshpajouhnejad, P., Hashmi, M. F., Bashir, K., & John, B. K. (2023). Acute Kidney Injury (Nursing). StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK568593/
- Kaplan Nursing. (2023). Alterations in Body Systems. NCLEX-RN Content Review Guide (9th ed.). Kaplan Test Prep.
- Kusumoto, F. (2020). ECG Interpretation: From Pathophysiology to Clinical Application (2nd ed.). Springer Nature.
- Silvestri, A. E., Grewal, A., & Gim, J. (2021). Saunders Comprehensive Review for the NCLEX-PN Examination (9th ed.). Elsevier.
- Tung, R. T. (2021). Electrocardiographic Limb Leads Placement and Its Clinical Implication: Two Cases of Electrocardiographic Illustrations. Kansas Journal of Medicine, 14, 229–230. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8415387/
The following links do not belong to Tecmilenio University, when accessing to them, you must accept their terms and conditions.
Readings
- Oxford Medical Education. (n.d.). ECG (EKG) Interpretation. https://oxfordmedicaleducation.com/ecgs/ecg-interpretation/
Videos
- RegisteredNurseRN. (2023, February 27). EKG Rhythms | ECG Heart Rhythms Explained - Comprehensive NCLEX Review [Video]. YouTube. https://www.youtube.com/watch?v=RoU4s18DXI4
- RegisteredNurseRN. (2023, February 27). 12 Lead ECG Placement of Electrodes | EKG Sticker Lead Procedure [Video]. https://www.registerednursern.com/ekg-12-lead-electrode-placement-ra-rl-la-ll-v1-v2-v3-v4-v5-v6/
La obra presentada es propiedad de ENSEÑANZA E INVESTIGACIÓN SUPERIOR A.C. (UNIVERSIDAD TECMILENIO), protegida por la Ley Federal de Derecho de Autor; la alteración o deformación de una obra, así como su reproducción, exhibición o ejecución pública sin el consentimiento de su autor y titular de los derechos correspondientes es constitutivo de un delito tipificado en la Ley Federal de Derechos de Autor, así como en las Leyes Internacionales de Derecho de Autor.
El uso de imágenes, fragmentos de videos, fragmentos de eventos culturales, programas y demás material que sea objeto de protección de los derechos de autor, es exclusivamente para fines educativos e informativos, y cualquier uso distinto como el lucro, reproducción, edición o modificación, será perseguido y sancionado por UNIVERSIDAD TECMILENIO.
Queda prohibido copiar, reproducir, distribuir, publicar, transmitir, difundir, o en cualquier modo explotar cualquier parte de esta obra sin la autorización previa por escrito de UNIVERSIDAD TECMILENIO. Sin embargo, usted podrá bajar material a su computadora personal para uso exclusivamente personal o educacional y no comercial limitado a una copia por página. No se podrá remover o alterar de la copia ninguna leyenda de Derechos de Autor o la que manifieste la autoría del material.