Physiological Adaptation / 06
Make sure to:
- Recall necessary knowledge to determine client needs derived from pathophysiological illness.
- Determine techniques and methods to assess the clients’ symptoms and parameters.
- Quote evidence-based nursing interventions to assist the client’s needs derived from pathologies.
 Health is the well-being of the body when it is in homeostasis, or in an adequate balance. This is achieved through the physiological functioning of the various body systems. Environmental factors or microorganisms can disrupt this homeostasis, interfering with the body's functioning and leading to diseases. The care needs depend on the client's pathology and how their body copes with this new condition. Nurses must identify these specific needs and be trained to provide comprehensive, quality care.
Health is the well-being of the body when it is in homeostasis, or in an adequate balance. This is achieved through the physiological functioning of the various body systems. Environmental factors or microorganisms can disrupt this homeostasis, interfering with the body's functioning and leading to diseases. The care needs depend on the client's pathology and how their body copes with this new condition. Nurses must identify these specific needs and be trained to provide comprehensive, quality care.
3.1 Applying Knowledge of Client Pathophysiology to Illness Management
 Pathologies, whether transmissible like the flu or HIV, or non-transmissible such as hypertension or diabetes, are significant factors in determining the necessary care for a patient. In both scenarios, understanding the progression of the pathologies is essential. This understanding includes knowing the possible causes, transmission mechanisms, risk factors, disease course, consequences, and possible adverse reactions to the disease or treatment.
Pathologies, whether transmissible like the flu or HIV, or non-transmissible such as hypertension or diabetes, are significant factors in determining the necessary care for a patient. In both scenarios, understanding the progression of the pathologies is essential. This understanding includes knowing the possible causes, transmission mechanisms, risk factors, disease course, consequences, and possible adverse reactions to the disease or treatment.
The natural history of a disease refers to its course when left untreated. During the pre-pathogenic period, the interaction between the agent, the host and the environment determines the disease’s form, including the mode of transmission, which is crucial for prevention. In the post-pathogenic period, the study focuses on when the disease’s causal agent affects the host and how the disease subsequently develops.
In transmissible diseases, there is a subclinical infection period after the agent enters the body, during which the patient does not exhibit symptoms. Usually, this period is an incubation period where the virus, bacteria, or fungus multiply.
Subsequently, a clinical horizon follows, in which the symptoms appear. During the prodromal stage, the first symptoms appear while the agent continues multiplying. The signs and symptoms continue in the illness stage, but the replication stage stops. Finally, the convalescence stage is the beginning of the recovery process. For non-transmissible diseases, the subclinical stage occurs in the absence of symptoms and is followed by the clinical horizon when symptoms appear.
A disease can be categorized as either acute (with a recent onset) or chronic (if it has lasted more than six months). Acute illnesses demand immediate attention and preparation of the patient, while chronic illnesses test patients' economic capabilities, resistance, and adherence to treatment.
Inflammation is a process that occurs in most pathologies to varying degrees. Signs of inflammation include pain, redness, swelling, heat, and warmth. After an injury, the skin recovery process is called wound healing, which has three stages: inflammation, proliferation, and remodeling. Inflammation is part of the initial body defense process, removing dead skin and activating the immune system to eliminate pathogens. The proliferation stage is the phase of re-epithelialization. Lastly, remodeling is the reorganization of the connective tissue (Malte et al., 2020)
The nursing holistic paradigm includes a personal and exhaustive assessment of the individual's biological, psychological, social, and spiritual needs. Patient education is an integral component of the nursing plan, addressing all knowledge deficits related to the specific health situation as part of an individualized educational process. Topics covered include the disease mechanism, risk factors, etiology, modes of transmission, mitigations, treatment options, strategies to achieve treatment adherence, possible effects of treatments, and alarm signs to return to the hospital, among others.
An IV line is essential in hospitalized patients for administering isotonic, hypertonic, or hypotonic solutions, and providing quick access to drug administration. IV gauges, ranging in sizes from 16-26, are used for all types of patients, depending on their specific needs. Smaller gauges, which are wider, allow for more fluid volume but require larger veins. The butterfly set, consisting of a needle measuring 0.5 to 1.5 inches in length and sizes ranging from 16-26, is particularly used in pediatric and geriatric patients.
Catheters are connected to IV tubing, which in turn connects to containers holding IV solutions made of glass or plastic. There are macrodrip (10-20 gt/ml) and microdrip (60 gt/ml) chambers to regulate the infusion of solutions. The microdrip is used in patients requiring meticulous fluid control, such as pediatric, geriatric patients, and those with fluid overload or receiving delicate medications like antibiotics. Intermittent infusion devices can also be useful for these purposes. For administering solutions like lipids, albumin, or blood derivatives, chambers equipped with filters are necessary to capture large molecules.
In hospitalized patients, the administration of hyperosmolar solutions, such as parenteral nutrition (PN), is essential. These lines are useful for measuring central venous pressure (CVP) or administering drugs. Placement involves using a sterile technique to introduce a large catheter via the femoral, jugular, or subclavian vein. The primary nursing care strategy is to prevent infections or coagulation of the catheter and to monitor the patient's hemodynamic state, especially after delivering any substances. Using the PN line exclusively is crucial.
The Broviac (or Groshong Hickman) catheters, used for long-term IV therapy, are inserted in the surgery room and managed with a sterile technique.
The Meiport Port-a-Cath, or Infusable port, is used for long-term administration of medications, such as chemotherapy. To use, one must first locate the device, and after asepsis and antisepsis, locate the port and insert the needle to administer the medication.
Remember to place the catheters using a sterile technique directed towards the heart. The most common location, as with IV cannulas, is the forearm, where the bones act as a natural splint. Secure the cannula with transparent dressings and record the placement date. Replace IV lines every 72-96 hours, change tubing every 96 hours, and change the dressing every 48 hours or as needed. Monitor the patient for complications such as air embolism, catheter embolism, fluid overload, electrolyte imbalance, infections, edema, hematoma, or burns (Silvestri & Silvestri, 2023c).
If signs of infection are detected (such as pain, redness, swelling, heat, warmth, purulent discharge, or fibrous material), check vital signs, notify the primary healthcare provider, remove the catheter, and send the catheter tip to the laboratory for culture. Collect blood from the catheter, prepare for hemoculture, record the body temperature and time. Monitor vital signs and prepare the patient for antibiotic administration.
The epidural catheter, used for administering analgesics, is inserted using a sterile technique. Before administering medication, aspiration is necessary. If blood or a transparent fluid is present, do not proceed and report it. Sensibility, movement, and perception of sensations need to be verified while the catheter is in place. If the fluid is cloudy or the patient has a fever, report it and prepare for antibiotic administration.
3.2 Unexpected Response to Therapies
 Monitoring vital signs is crucial for tracking a patient's recovery from baseline to the current moment. If significant changes occur, it indicates a need for immediate reporting to the multidisciplinary team to address all potential causes. Patients should be assessed in all dimensions: physical, psychological, social, and spiritual.
Monitoring vital signs is crucial for tracking a patient's recovery from baseline to the current moment. If significant changes occur, it indicates a need for immediate reporting to the multidisciplinary team to address all potential causes. Patients should be assessed in all dimensions: physical, psychological, social, and spiritual.
In the initial assessment, determining the patient's health status and evaluating the condition of body organs, it is necessary to assess neurological status, skin appearance, and renal health.
The first thing to do to determine a patient’s general health status and evaluate the general condition of the body organs, it is necessary to assess the neurological status, skin appearance, and renal state of health.
Neurological status can be assessed using the Glasgow Coma Scale (GCS). The maximum score of 15 indicates optimal conditions, while lower scores suggest a worsening health condition.
Table 1
Glasgow Coma Scale
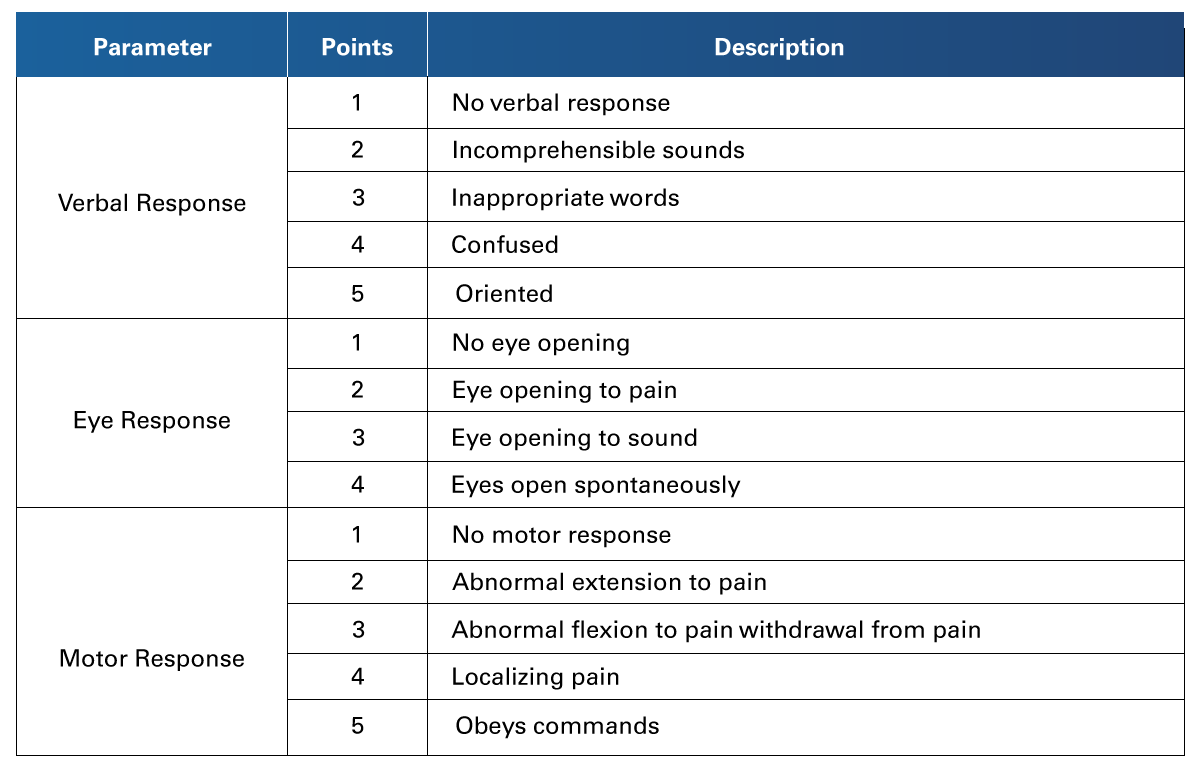 Retrieved from Jain, S., & Iverson, L. (2023). Glasgow Coma Scale. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK513298/
Retrieved from Jain, S., & Iverson, L. (2023). Glasgow Coma Scale. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK513298/
Evaluating the skin by assessing capillary refill helps determine the state of distal perfusion. A pale appearance may indicate blood loss or anemia, while marbled, diaphoretic, and cold skin suggest shock.
To evaluate kidney function, calculate enuresis at 0.5 ml/kg (Goyal et al., 2023). Decreased urine output indicates a need for the body to compensate for homeostasis due to reasons such as hypovolemia, hypotension, shock, or other emergencies.
Any alterations in the parameters must be communicated to the multidisciplinary team for prompt attention.
In cases of anaphylactic reactions to treatment or impairment due to life-threatening medical conditions, emergency patient care includes ABCDE actions: Airway permeability, Breath control and oxygenation as required, Circulation control including hemorrhage management and cardiac monitoring, Neurological Deficit identification, and Examination and Exposure to identify causes, signs, or symptoms (American Heart Association, n.d).
Nursing diagnoses, including risk of falls and risk of infection, should also be considered.
3.3 Managing the Care of a Client with Impaired Ventilation/Oxygenation
 Oxygenation is a vital bodily function. Any variation in its quality can lead to tissue injuries, potentially resulting in cell death, gangrene, and systemic failure.
Oxygenation is a vital bodily function. Any variation in its quality can lead to tissue injuries, potentially resulting in cell death, gangrene, and systemic failure.
Some known risk factors for respiratory disorders are smoking, viral respiratory diseases, chest injury, surgery, allergies, and exposition to irritant substances.
Signs of impaired respiration include dyspnea, tachypnea, bradypnea, irritability, pale or cyanotic skin, slow capillary refill, lethargy, and unconsciousness. The Silverman-Anderson Score evaluates five parameters of infant breathing effort: upper chest movement, lower chest retraction, xiphoid retraction, nares dilation, and expiratory grunt. A score of 0 indicates comfortable breathing, while a 10 indicates severe respiratory distress. Nurses must monitor all vital signs, especially heart rate, respiratory rate, and SaO2, to properly track a patient's ventilation and oxygenation status.
Oxygen is administered in a precise dose, dependent on the current response. It's crucial to remember that administering less oxygen than required can lead to hypoxia, while excessive oxygen can cause alkalosis (Hardavella et al., 2019).
The composition of environmental air is 21% oxygen, known as the Fraction of Oxygen (FIO2). Low oxygen flows are provided to relatively stable patients using devices like nasal cannulas, which deliver FIO2 of 24-40% at 1 to 6 L/min. Simple face masks provide FIO2 of 35-55%, and non-rebreather masks deliver 85-95% at 10-15 L/min.
Devices for high flux are used in more complex patients, mostly patients on pre-hospital care or ER rooms, to provide fast stabilization. These are: the rebreather mask, with a FIO2 of 70%, and the Venturi mask with 24-50%. Nurses must be familiar with these devices to provide the correct device and oxygen flux according to the patient’s needs.
More definitive equipment includes an endotracheal cannula and an endotracheal tube.
Another useful blood laboratory test is the arterial blood gas test. This test is conducted using a heparinized insulin syringe to draw blood from an artery, and it should be processed promptly, recording the body temperature and time. Normal values are presented in Table 2.
Table 2
Arterial Blood Gas Values and Interpretation
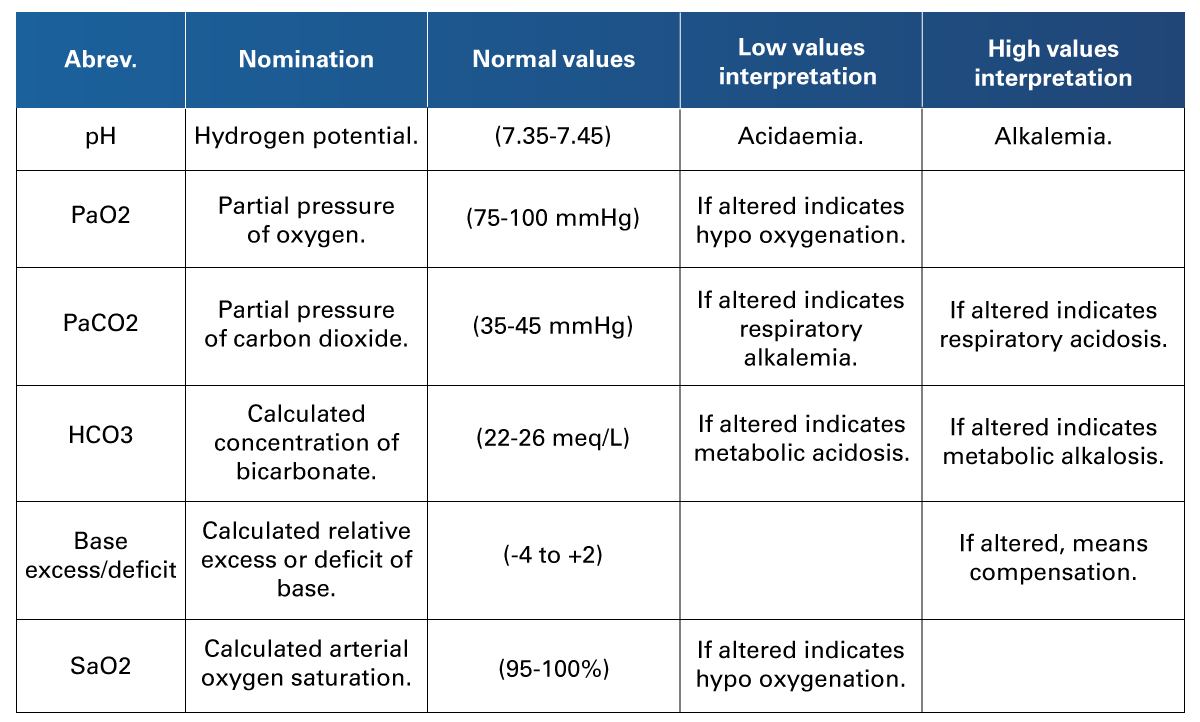 Adapted from Cid-Juárez et al. (2023). Arterial Blood Gases in Normal Subjects at 2240 Meters Above Sea Level: Impact of Age, Gender, and Body Mass Index. Clinical Research Magazine. 75(1).
Adapted from Cid-Juárez et al. (2023). Arterial Blood Gases in Normal Subjects at 2240 Meters Above Sea Level: Impact of Age, Gender, and Body Mass Index. Clinical Research Magazine. 75(1).
Nurses may be involved in other studies or procedures for patients with respiratory issues, such as sputum culture, laryngoscopy, bronchoscopy, thoracentesis, lung biopsy, tuberculin skin test, and invasive mechanical ventilation.
The sputum culture involves the collection of sputum from expectoration or tracheal suctioning to study the presence of the microorganisms. One method is instructing the patient to force a cough and to place the second sputum on a sterile recipient during the first hours of the morning without washing the teeth or having breakfast. The other method is doing an aspiration of secretions with a sterile technique and placing 15 ml of them on a sterile recipient. This type of study used to be on a series of three continuous days (Silvestri & Silvestri 2023a).
Laryngoscopy and bronchoscopy are studies conducted with a fiberoptic bronchoscope to internally observe the airway. The patient is instructed to keep the mouth clean and free of any objects, including artificial dentures. The nurse administers local anesthesia spray, instructing the patient not to swallow it, and installs IV lines for access to medications or sedation. It is crucial to remember not to measure blood pressure at the site used for IV medication for the next 24 hours (Silvestri & Silvestri, 2023a).
Thoracentesis is a procedure to remove fluid, blood, or air trapped between the pleural layers. The patient is seated on the bed or lies down on the affected side. The nurse performs asepsis and antisepsis, and after the procedure, applies a pressure dressing and monitors the patient's progress (Silvestri & Silvestri, 2023a).
A lung biopsy is the extraction of lung tissue to examine the cells. Nursing procedures are similar to those for thoracentesis, except that anesthesia or other pain medications may be indicated in this case (Silvestri & Silvestri, 2023a).
The tuberculin skin test involves injecting Bacille Calmette-Guérin (BCG) into the upper third of the inner surface of the left arm. After the injection, the site is marked, and the reaction is measured 48-72 hours later to determine if it is positive (Silvestri & Silvestri, 2023a).
Invasive mechanical ventilation (IMV) automatically controls oxygenation and respiration, temporarily providing positive pressure through a tube into the airway, via a mask-valve bag, and, if needed, a ventilator. The endotracheal tube is introduced through the mouth and placed just above the junction of two bronchi. It is secured at the mouth to maintain its position. This procedure may require sedation or other medications. Nurses must ensure a patent IV line and prevent accidental extubation. To verify the tube's correct placement, CXR (chest x-ray), ultrasonography, and EtCO2 waveform are performed (Silvestri & Silvestri, 2023a).
3.4 Providing Ostomy Care and Education
 Ostomies are surgical procedures where a portion of the intestine is brought out through the skin, creating an opening for feces elimination and allowing the distal portion of the intestine to rest. The ostomy's name varies with its location, including ileostomy, ascending colostomy, transverse colostomy, descending colostomy, and sigmoid colostomy.
Ostomies are surgical procedures where a portion of the intestine is brought out through the skin, creating an opening for feces elimination and allowing the distal portion of the intestine to rest. The ostomy's name varies with its location, including ileostomy, ascending colostomy, transverse colostomy, descending colostomy, and sigmoid colostomy.
During the pre-operative period, confirming the procedure details through the surgical order, informed consent, and relevant laboratory tests, such as coagulation studies, blood type, and hematological parameters, is essential. Additionally, prescribing fasts, laxatives, enemas, and antibiotics may be necessary to manage bacterial content.
After surgery, monitoring the skin's integrity is crucial for detecting signs of gangrene, irritation, or infection. The expected skin color in these situations is red. Pale skin may indicate anemia, pearl color suggests infection, and obscure tones might indicate an absence of perfusion. The borders should be clearly defined and securely attached to the skin to minimize the risk of intrusion (Silvestri & Silvestri, 2023b).
The ostomy's proximity to the small intestine affects stool consistency, with more proximal ostomies producing liquid and acidic stool. Thus, maintaining the patient's skin integrity is crucial. Applying physical protective barriers, like ointments, and timely emptying the collection bag before it reaches the skin (particularly when contents are in the bag's second third) are essential. Regular irrigation of the ostomy ensures hydration and cleanliness. Preserving skin integrity and preventing infections are vital aspects for overall patient well-being.
 In conclusion, the needs and demands of each patient are unique because they depend on the general state of health, the pathology and the interventions carried out with each patient. Nurses must be prepared to meet the various needs, so it is essential to understand aspects of physiology, pathology, procedures, materials and equipment to provide comprehensive, quality care.
In conclusion, the needs and demands of each patient are unique because they depend on the general state of health, the pathology and the interventions carried out with each patient. Nurses must be prepared to meet the various needs, so it is essential to understand aspects of physiology, pathology, procedures, materials and equipment to provide comprehensive, quality care.
- American Heart Association. (n.d.). Algorithms. https://cpr.heart.org/en/resuscitation-science/cpr-and-ecc-guidelines/algorithms
- Cid-Juárez, S., Téllez-Navarrete, N. A., Bautista-Bernal, A., León-Gómez, P., Salas-Escamilla, I., Gochicoa-Rangel, L., & Pérez-Padilla, R. (2023). Arterial Blood Gases in Normal Subjects at 2240 Meters Above Sea Level: Impact of Age, Gender, and Body Mass Index. Clinical Research Magazine, 75(1), 29-36.
- Goyal, A., Daneshpajouhnejad, P., Hashmi, M. F., Bashir, K., & John, B. K. (2023). Acute Kidney Injury (Nursing). StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK568593/
- Hardavella, G., Karampinis, I., Frille, A., Sreter, K., & Rousalova, I. (2019). Oxygen Devices and Delivery Systems. Breathe, 15(3), e108–e116. https://doi.org/10.1183/20734735.0204-2019
- Jain, S., & Iverson, L. (2023). Glasgow Coma Scale. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK513298/
- Malte, B. N., Glatz, M., & Proksch, E. (2020). Optimal Support of Wound Healing: New Insights. Dermatology, 236(6), 593–600. https://doi.org/10.1159/000505291
- Silvestri, L. A., & Silvestri, A. E. (2023a). Urinary and Bowel Elimination. Saunders Comprehensive Review for the NCLEX-PN Examination (9th ed.). Elsevier. 218-233.
- Silvestri, L. A., & Silvestri, A. E. (2023b). Respiratory Problems of the Adult Client. Saunders Comprehensive Review for the NCLEX-PN Examination (9th ed.). Elsevier. 679-700.
- Silvestri, L. A., & Silvestri, A. E. (2023c). Complex Care. Saunders Comprehensive Review for the NCLEX-PN Examination (9th ed.). Elsevier. 1015-1089.
The following links do not belong to Tecmilenio University, when accessing to them, you must accept their terms and conditions.
Readings
- Castro, D., Patil, S. M., & Keenaghan, M. (2024, Janaury 8). Arterial Blood Gas. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK536919/
Videos
- NURSINGcom w/Jon Haws, RN. (2021, October 27). Stoma Care - Changing a Colostomy Bag (Nursing Skills) [Video]. YouTube. https://www.youtube.com/watch?v=_K4phsNsy5U
La obra presentada es propiedad de ENSEÑANZA E INVESTIGACIÓN SUPERIOR A.C. (UNIVERSIDAD TECMILENIO), protegida por la Ley Federal de Derecho de Autor; la alteración o deformación de una obra, así como su reproducción, exhibición o ejecución pública sin el consentimiento de su autor y titular de los derechos correspondientes es constitutivo de un delito tipificado en la Ley Federal de Derechos de Autor, así como en las Leyes Internacionales de Derecho de Autor.
El uso de imágenes, fragmentos de videos, fragmentos de eventos culturales, programas y demás material que sea objeto de protección de los derechos de autor, es exclusivamente para fines educativos e informativos, y cualquier uso distinto como el lucro, reproducción, edición o modificación, será perseguido y sancionado por UNIVERSIDAD TECMILENIO.
Queda prohibido copiar, reproducir, distribuir, publicar, transmitir, difundir, o en cualquier modo explotar cualquier parte de esta obra sin la autorización previa por escrito de UNIVERSIDAD TECMILENIO. Sin embargo, usted podrá bajar material a su computadora personal para uso exclusivamente personal o educacional y no comercial limitado a una copia por página. No se podrá remover o alterar de la copia ninguna leyenda de Derechos de Autor o la que manifieste la autoría del material.